Research

Research

Research

What we do
What we do
Lung Organoids
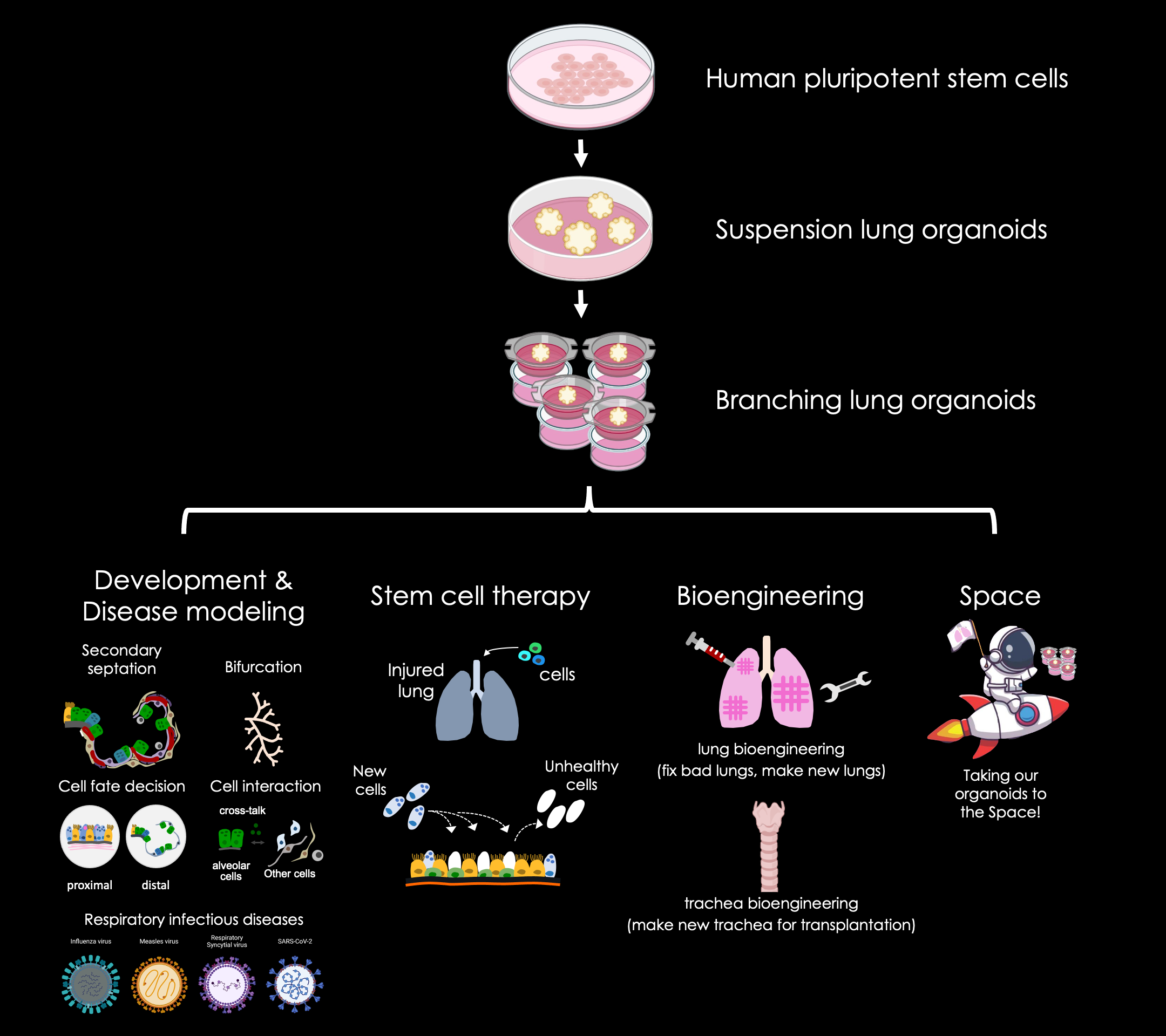
We use lung organoids as a model to study lung development and lung diseases in the lab. Lung organoids are miniature lungs in a dish we generate from human pluripotent stem cells in the lab. Human pluripotent stem cells are cells that theoretically can give rise to all cells of the body.
Respiratory Infectious Disease Modeling
Responding to infectious disease caused by coronavirus family and influenza virus requires access to human model systems that recapitulate disease pathogenesis, reveal potential targets, and enable drug testing. A particular priority is access to primary human lung in vitro model systems, with the variety of respiratory epithelial cells that are the proposed targets of viral entry. The lung organoid system provides a more accurate depiction of cell behavior and represents tissues better than conventional cell lines, and offers less complexity than tissue explants or animal models. We have used the lung organoid model successfully modeling several respiratory infectious disease, such as SARS-CoV-2, respiratory syncytial virus, measles, and influenza. The lab is focusing on finding a way fighting SARS-CoV-2 and influenza viral entries.
Respiratory Infectious Disease Modeling
Responding to infectious disease caused by coronavirus family and influenza virus requires access to human model systems that recapitulate disease pathogenesis, reveal potential targets, and enable drug testing. A particular priority is access to primary human lung in vitro model systems, with the variety of respiratory epithelial cells that are the proposed targets of viral entry. The lung organoid system provides a more accurate depiction of cell behavior and represents tissues better than conventional cell lines, and offers less complexity than tissue explants or animal models. We have used the lung organoid model successfully modeling several respiratory infectious disease, such as SARS-CoV-2, respiratory syncytial virus, measles, and influenza. The lab is focusing on finding a way fighting SARS-CoV-2 and influenza viral entries.
Cell Fate Decision
The discovery of hPSCs laid the foundation for an emerging field of biomedical research that holds promise for developing models of human development and disease, establishing new strategies for discovering and testing drugs, and providing systems for generating cells and tissues for transplantation. Although the potential of hPSCs is truly outstanding, fulfilling this potential depends on our ability to efficiently generate functional cell types from them. One of the key problems in the stem cell directed differentiation field is that we are able to efficiently generate alveolar epithelial type II (AT2) cells but cannot efficiently generate alveolar epithelial type I (AT1) cells. On the contrary, it is nearly impossible to keep primary AT2 cells transdifferentiating to AT1 cells after isolating and culturing the cells. We have recently discovered a factor that can delay transdifferentiation from AT2 cells to AT1 cells. By identifying and revealing the mechanism of the factor, we will potentially have a tool to specifically generate AT1 or AT2 cells.
Stem Cell Therapy
In the field of regenerative medicine, one of the biggest challenges is regenerating organs comparable to the originals that form during embryonic development. When a human organ is injured or amputated, it does not form the regeneration bud that is required to regrow the damaged organ. In some severe lung diseases, pneumonectomy/lobectomy is necessary to improve a patient’s quality of life. However, once removed, human lungs do not regenerate. In our lab, we are exploring the potential of using lung organoids as the regenerative bud for lung regeneration.
Stem Cell Therapy
In the field of regenerative medicine, one of the biggest challenges is regenerating organs comparable to the originals that form during embryonic development. When a human organ is injured or amputated, it does not form the regeneration bud that is required to regrow the damaged organ. In some severe lung diseases, pneumonectomy/lobectomy is necessary to improve a patient’s quality of life. However, once removed, human lungs do not regenerate. In our lab, we are exploring the potential of using lung organoids as the regenerative bud for lung regeneration.
Trachea Transplantation
With few definitive treatment options available, tracheal transplantation is widely proposed for patients suffering end-stage upper airway diseases. However successful tracheal transplantation surgery remains a major challenge in the field of thoracic surgery and regenerative medicine. Previous trials in patients had shown that recellularization (re-cell) of the tracheal scaffold is crucial to obtain functional long-segment tracheal grafts. Grafts without substantial epithelial cell coverage uniformly fail to remodel appropriately and lead to graft failure. One of the biggest hurdles to successful creation of tissue-engineered tracheas is an inability to isolate and expand a sufficient number of epithelial cells from patients for re-cell. For the past two years, we have developed a method that enables us to expand basal cells, the stem cell of the airways, in vitro from human pluripotent stem cells. The immediate application is to serve as an unlimited source of cells for tissue-engineered tracheal/airway reconstruction. We are evaluating the potential of the stem cell-generated basal cells to serve as an unlimited epithelial cell source for tracheal/airway reconstruction and to create a bioengineered tracheal graft with functional epithelium.
Injury models
To study the mechanism of injury and repair in the distal lung, we have created injury models using lung organoids. We induce different levels of damage or cell death in the lung organoids to study injury and repair.
Injury models
To study the mechanism of injury and repair in the distal lung, we have created injury models using lung organoids. We induce different levels of damage or cell death in the lung organoids to study injury and repair.