WHAT IS AUTONOMIC FUNCTION TESTING FOR?
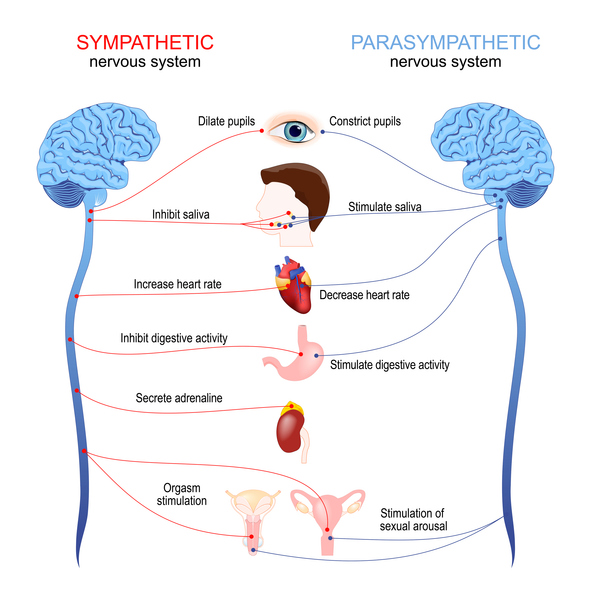
Autonomic function tests, AFTs, evaluate how well the autonomic nervous system is functioning. The autonomic nervous system regulates bodily functions that don’t require conscious control, processes such as heart rate, blood pressure, and digestion. An AFT is an instrumental component in diagnosing conditions that affect autonomic functions and result in symptoms such as dizziness, fainting, or weakness. A patient’s provider may recommend an AFT if they report specific unexplained symptoms or suspect that they have specific chronic conditions. During the test, the research technicians will monitor how a patient’s blood pressure and heart rate respond to certain challenges and stimuli.
COMPONENTS OF THE TEST
An AFT is comprised of 4 parts: quantitative sudomotor axon reflex test (QSART), Heart Rate Deep Breathing (HRDB) exercise, Valsalva maneuver, and the tilt table test.
QSART
To perform the QSART, which measures sweat output, the research technician attaches four plastic capsules to a patient’s left arm and leg and fills these capsules with a liquid that causes sweating. The capsules are also attached to a battery that sends a small amount of electricity through the liquid, usually accompanied by a slight pricking sensation, which allows us to measure their sweat response.


HRDB & VALSALVA
The next two exercises are the cardiovagal tests included in the AFT procedure. To evaluate how a patient’s heart rate and blood pressure respond to changes in their breathing pattern, we put the following equipment onto their body: electrocardiogram stickers attached to wires on their chest and cuffs on their fingers and arms. The finger cuff fills with air and squeezes their fingers consistently throughout the next 3 exercises. The HRDB exercise involves taking 8 slow, deep breaths and the Valsalva maneuver involves exhaling hard into a tube for 15 seconds.
TILT TABLE
The tilt table test is the final portion of the AFT, in which changes in a patient’s blood pressure and heart rate are monitored while they experience a change in position. After a 5-minute period of lying flat on a table, the table tilts upwards until the patient is almost completely upright, keeping them standing at an 80-degree angle. Patients are urged to tell the technician if they feel any symptoms during this portion of the tilt, including, but not limited to lightheadedness, nausea, and heaviness in their lower extremities. If a patient does not experience any significant symptoms, they will remain there for 10 minutes total and then return to a supine position where they will be monitored for 5 more minutes.
WHAT DO THE RESULTS MEAN?
The test results are analyzed by Dr. Robinson-Papp and Dr. Mueller who look at patients’ sweat response rates, changes in heart rate and blood pressure, and respiratory rate to find any potential abnormalities in their autonomic nervous system. Your referring doctor should discuss the results of the test with you.
Qsweat is the commercial version of QSART (which is no longer used), this is only important because the normal values are different. Sweat testing reflects the function of the small sympathetic fibers innervating the sweat glands. If sweating is reduced it could mean that these fibers are not functioning properly, but this can also happen if there are local abnormalities in the skin. Also, many common medications can reduce sweat output. Therefore, if QSweat is reduced and this is the only abnormality we often do not consider this very significant. Normal Qsweat means these fibers are functioning normally but does not exclude an autonomic disorder involving the central nervous system. High sweat output does not have any known clinical significance.
The other three tests all assess cardiovascular autonomic reflexes. It is the job of these reflexes to keep BP stable in response to perturbation by 1) changing the heart rate (HR), this HR variability reflects primarily parasympathetic (aka vagal) function; 2) changing the amount of constriction in the blood vessels, which relies on sympathetic function.
In the Valsalva maneuver, the patient is asked to blow out forcibly into a tube. Doing so increases pressure in the chest and transiently impedes venous blood flow back to the heart causing BP to fall. If the parasympathetic (aka vagal) part of the ANS is working well heart rate will rise to arrest the fall in BP. The Valsalva ratio is the ratio of the highest to lowest HR observed in the test. There is an age-adjusted cut-off for the lower limit of normal. There is no upper limit of normal. We also may comment if the BP falls much more than expected since this may indicate a problem in sympathetic function.
In heart rate response to deep breathing, we measure heart rate variability during a standardized deep breathing task. Normally this task causes the HR to rise and fall with the breath, this is mediated by the parasympathetic (aka vagal) system. There is an age-adjusted cut-off for the lower limit of normal. There is no upper limit of normal.
In the tilt table test we observe the HR and BP as the patient goes from a supine to upright position. This movement causes blood to pool briefly in the legs. A normal sympathetic nervous system will compensate for this quite quickly by constricting those blood vessels and so often no change in HR or BP is observed. It is also normal to see a small increase in HR and/or fall in BP. It is abnormal if there is a sustained decrease of at least 20 mmHg in systolic BP and/or 10 mmHg in diastolic BP. It can also be abnormal if BP rises during the tilt although a threshold for abnormality is not defined. A sustained increase in HR of >30 BPM (in adults) is also considered abnormal.
PAIRED Project
paired.project@mssm.edu
212-241-0190