By Jessica Robinson-Papp, MD MS
Last month we were excited to have a new manuscript published online in the Journal of Neuroimmune Pharmacology exploring how dysfunction of the autonomic nervous system (ANS) might impact immune function. It’s been known for a long time that the sympathetic nervous system sends nerve fibers into all the organs of the immune system. This includes so-called “primary lymph organs” like the thymus and the bone marrow where immune cells are born, and “secondary lymph organs” like the lymph nodes and spleen where immune cells congregate. It’s also known that immune cells have specialized receptors for norepinephrine, the neurotransmitter released by sympathetic nerve fibers, and that immune cells change their behavior in response to norepinephrine. But hardly any of this research has been done in humans, probably because it’s difficult (if not impossible) to directly image or measure the activity of these tiny nerves deep inside the human body.
At the PAIRED Project we use a battery of autonomic function tests (check out a video of alum, Alyha Benitez, demonstrating) to approximate the function of the ANS and rate it on a simple 0-10 scale called the Composite Autonomic Severity Score (CASS). For this new study, we divided research participants into four groups based on their CASS score. We then measured a panel of 41 cytokines in their blood. These cytokines are substances produced by immune cells that have complex effects on the body. Ideally, they help coordinate the fight against infection, but when not properly regulated they can cause damage through excessive inflammation. The figure below is the main finding from the study which shows four different cytokine networks, one for each of the four groups of participants.
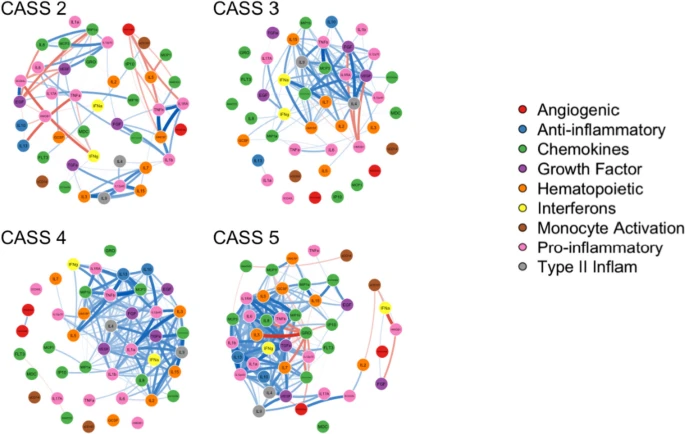
In the network each circle represents one cytokine, and a blue connector between the circles indicates a positive correlation. Positive correlation means they tend to do the same thing, like if the level of one cytokine is high in a participant, then so is the level of the connected cytokine. The differences between the networks are visually striking: the networks with higher CASS scores are much bluer, much more strongly connected. This means that in the higher CASS groups (i.e., the people with worse autonomic function) patients’ cytokines tend to exhibit an “all or nothing” response. In a kind of “mob mentality,” if one cytokine is low, they all tend to be low, and if one cytokine is high, they all tend to be high.
Why might this be? Perhaps a normal ANS, with its nerve fibers reaching into the places where immune cells reside, instructs those cells on what cytokines to release, allowing for an appropriately restrained immune response when a threat is detected. If that’s true, then loss of these nerve fibers might result in an overzealous less-targeted response to threat. A normal ANS might also be responsible for assessing the threat level in the first place through its sensory branches, and so an immune system without this neurologic control system may be both blind and bellicose.
These are still early findings, and a lot of work remains. This study examined cytokines, which are released from immune cells, but we didn’t examine the immune cells themselves. We also used the CASS as a summary score of autonomic function, but we still don’t have a good way of specifically measuring the nerve fibers innervating lymph nodes and other immune organs. These are puzzles still to be worked out as we seek to expand our understanding of neurologic control of immunity.