If you live with a chronic pelvic pain disorder (CPPD), you’ve probably noticed something: your period can make everything worse. The pain intensifies and sometimes spreads to new places. Suddenly you’re dealing with bloating, digestive issues, and a whole constellation of symptoms that seem to arrive right on schedule (!).
Today, we are sharing some observations from the very data dashboard of our data wizard-in-residence, Samia, as we continue to analyze the data from our CPP Tracker study. The visualizations reveal striking patterns comparing participants with and without CPPDs and support what so many have experienced but struggled to quantify: periods don’t just add pain for people with CPP—they amplify what’s already there. So here they come, straight from Samia’s dashboard to your screen.
The Numbers Don’t Lie: Period Days Hit Different
Let’s start with the most striking finding. Among our participants with CPPDs, 83.8% of period days involved pain. That’s more than 8 out of 10 days during menstruation.
Compare that to those without CPPDs: just 12% of their period days involved pain.
But wait—you might be thinking—people with CPPDs experience pain on non-period days too, right? Absolutely. The data indicate that 75.3% of non-period days involved pain for the CPPDs group. So yes, pain is a constant companion, and period pain days are consistently amplified. Take a look at the comparison below—the difference between the two groups of participants tells this story.
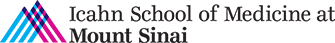
It’s Not Just More Pain—It’s Worse Pain
The frequency data tells one story, but severity tells another. When we looked at how intense the pain was on period days versus non-period days, a clear pattern emerged.
If you look at the baseline pain levels above, you can see something interesting: off period; those with CPPDs show less day-to-day variability—their pain stays at a fairly consistent level. Those without CPPDs, on the other hand, have much more variability in their pain.
But here’s the key finding: during periods, those with CPPDs consistently experience higher pain severity than those without CPPDs. For those without CPPDs, those occasional period pain spikes stand out sharply because their pain baseline is so much lower. For people with CPPDs, though, it’s not just a spike—the entire pain floor gets elevated.
This isn’t just “normal period cramps on top of existing pain.” For people with CPPDs, menstruation significantly increases the pain experience.
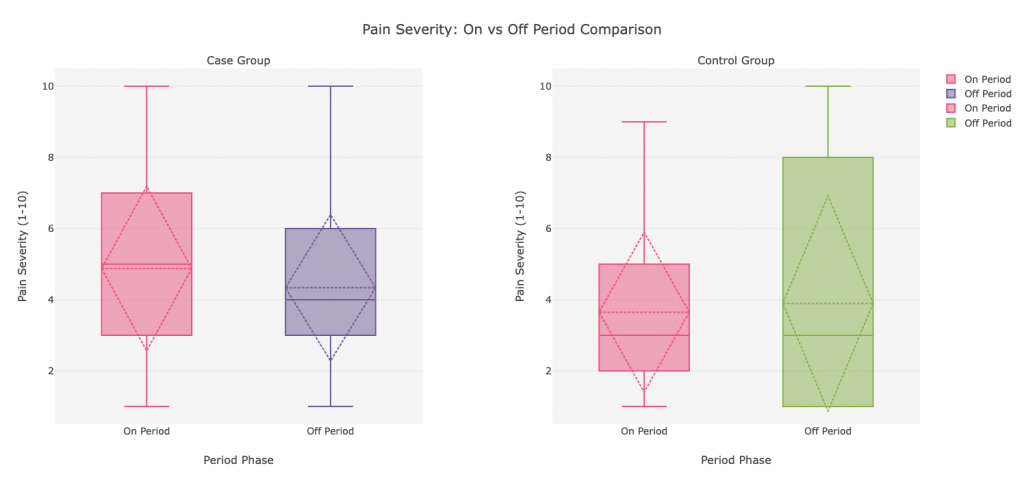
Your Pain Has a Geography (And It Changes with Your Cycle)
Pain doesn’t exist in abstract—it shows up in specific places. And those places matter.
Lower back and pelvis were the VIPs of period pain for our CPP participants, showing up on nearly half of period days. But here’s what’s fascinating: abdomen, hip, and vaginal pain all increased during menstruation too. When viewing the chart above, you can see that for those without CPPD, the pain they have off period in these locations is quite low, whereas if you look at their pain during their period there is a large “jump” in those locations. Compared to those without a CPPD diagnosis, participants with a CPPD who have ongoing pain see an increase, but their baseline of pain when they are not on their periods is so much higher.
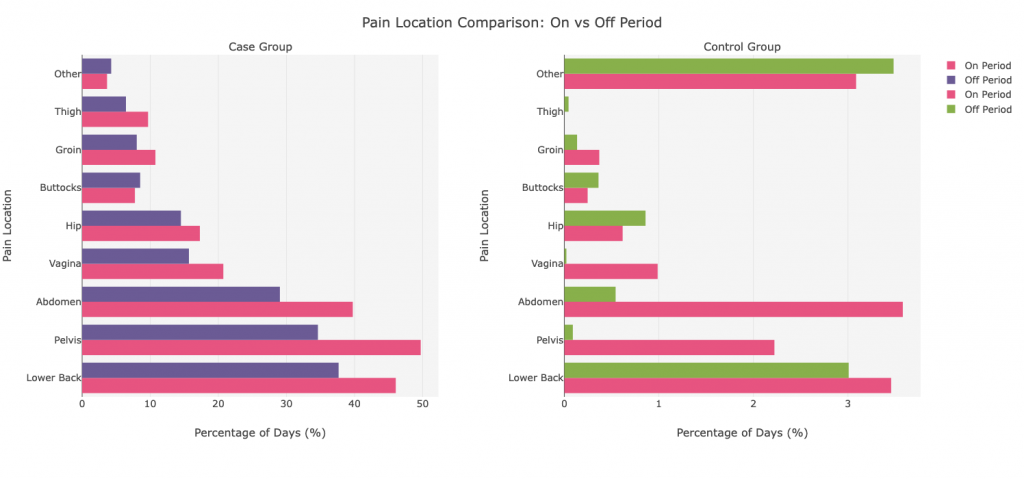
The Symptom Cascade: When Pain Brings Friends
As if increased pain wasn’t enough, a visual inspection in our data dashboard reveals that periods often trigger a cascade of other symptoms. Digestive and urinary issues that might be manageable during non-period days intensify, too.
Bloating led the charge, affecting over 40% of period days in the CPP group. Gas, constipation, and abdominal pain weren’t far behind. These aren’t separate issues—they’re part of the same story; all interconnected through the complex web of pelvic anatomy and nervous system sensitivity.1
Again, those without CPPD experienced these symptoms far less frequently, and the difference between their period and non-period days was smaller.
Why This Matters
If you’re reading this and nodding along, recognizing your own experience in these charts—that’s exactly the point. For too long, people with CPP have been told their period pain is “normal” or that they’re overreacting. These data say otherwise.
Understanding these patterns helps us in several ways:
- It validates patient experiences with objective data
- It helps clinicians recognize that menstrual phase matters in CPP management
- It guides research into why periods amplify pain and how we might intervene
Your experience is real, it’s measurable, and it’s different from typical period discomfort. The data see what you’ve been feeling all along.
References.
- Choung RS, Herrick LM, Locke GR 3rd, Zinsmeister AR, Talley NJ. Irritable bowel syndrome and chronic pelvic pain: a population-based study. J Clin Gastroenterol. 2010;44(10):696-701. doi:10.1097/MCG.0b013e3181d7a368