Cognitive Psychophysiology Lab
Dr. Hazlett’s multidisciplinary and translational research utilizes neuroimaging and other psychophysiological measures to study normal and disordered cognition and emotion. Her laboratory’s multi-measure approach employs functional brain imaging (e.g., functional magnetic resonance imaging) together with more basic psychophysiological measures (e.g., skin conductance responsivity and modulation of the startle eye-blink response) to investigate and characterize information-processing deficits in schizophrenia-spectrum disorders (e.g., schizophrenia, schizotypal personality disorder) and affective processing deficits in personality disorders (e.g., borderline personality disorder) and major depression characterized by emotion dysregulation. Functional brain imaging allows a window onto the brain’s activity while the more basic psychophysiological measures allow superior temporal resolution (in milliseconds) to examine the magnitude and time course of the cognitive- and emotion-processing deficits observed in patients with various types of psychiatric illness. Dr. Hazlett is particularly interested in individual differences in attentional and emotional information processing that might predict treatment response.
Moreover, Dr. Hazlett has a long-standing interest in the clinical symptom and cognitive correlates of structural MRI abnormalities in the schizophrenia spectrum. She and her team are currently working on a five-year longitudinal study at Mount Sinai funded by the National Institutes of Mental Health that uses fMRI and neurocognitive assessments across the schizophrenia spectrum.
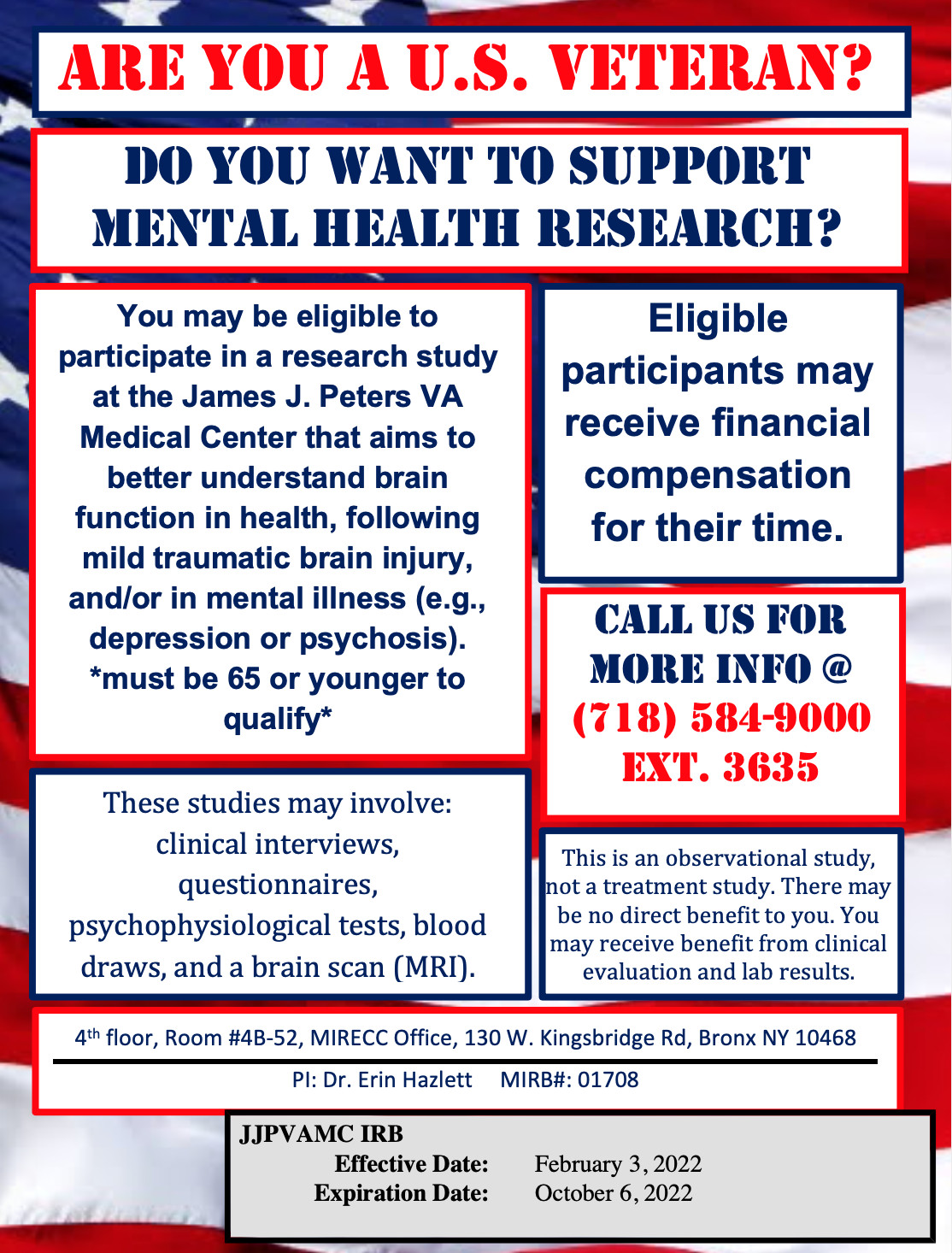
Finally, at the James J. Peters Department of Veterans Affairs Medical Center (a Mount Sinai affiliate), Dr. Hazlett is currently working on several VA Merit grants examining the neurobiology of suicidal behavior in military veterans.
Lab Director: Erin Hazlett, PhD, Psychiatry
Education
BA in Psychology, University of California, Los Angeles
MA in Psychology, University of Southern California
PhD in Psychology, University of Southern California
Biography
Dr. Hazlett is a Professor in the Department of Psychiatry and Director of the Cognitive Psychophysiology Laboratory. She is also a member of the Department of Neuroscience Training Faculty.
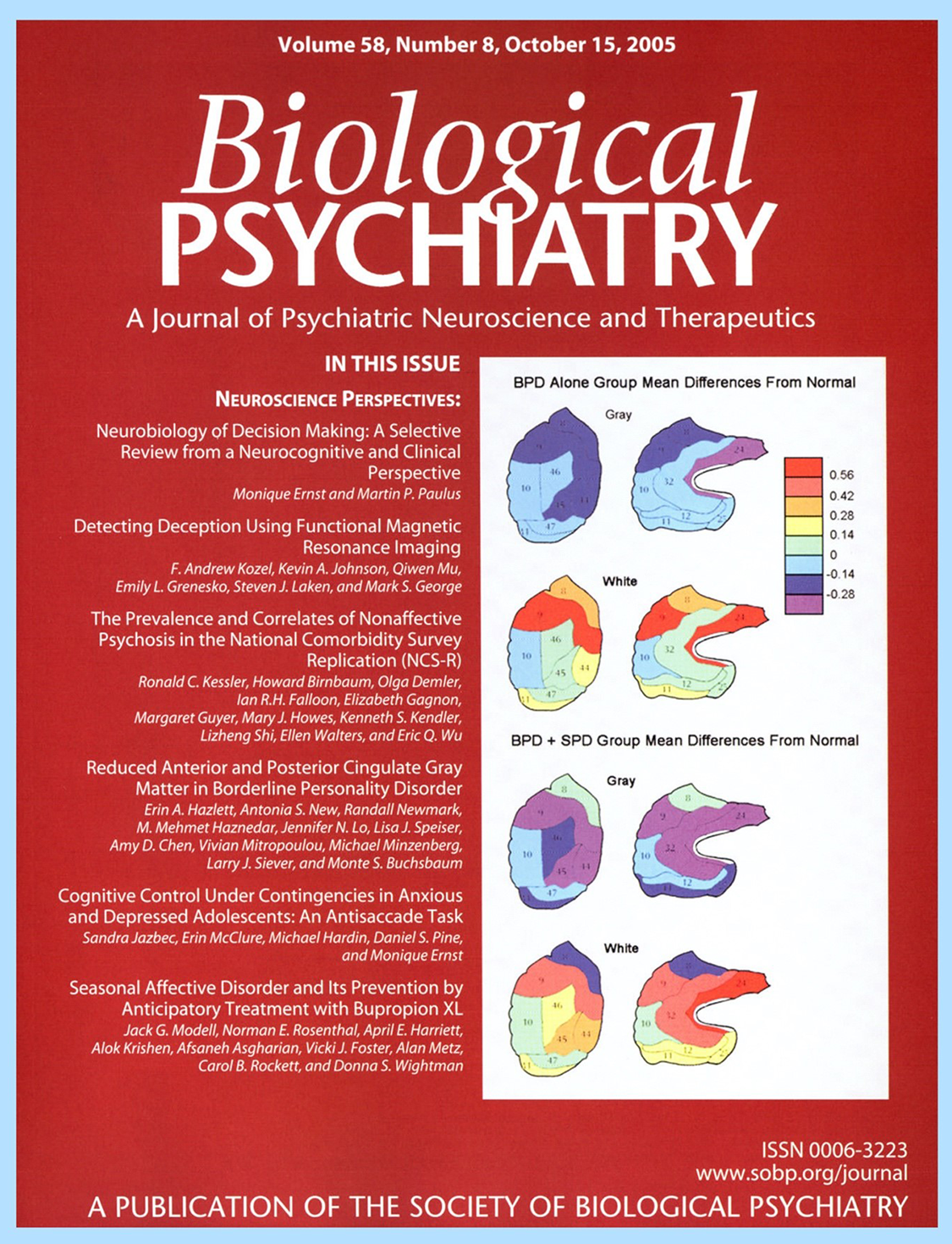
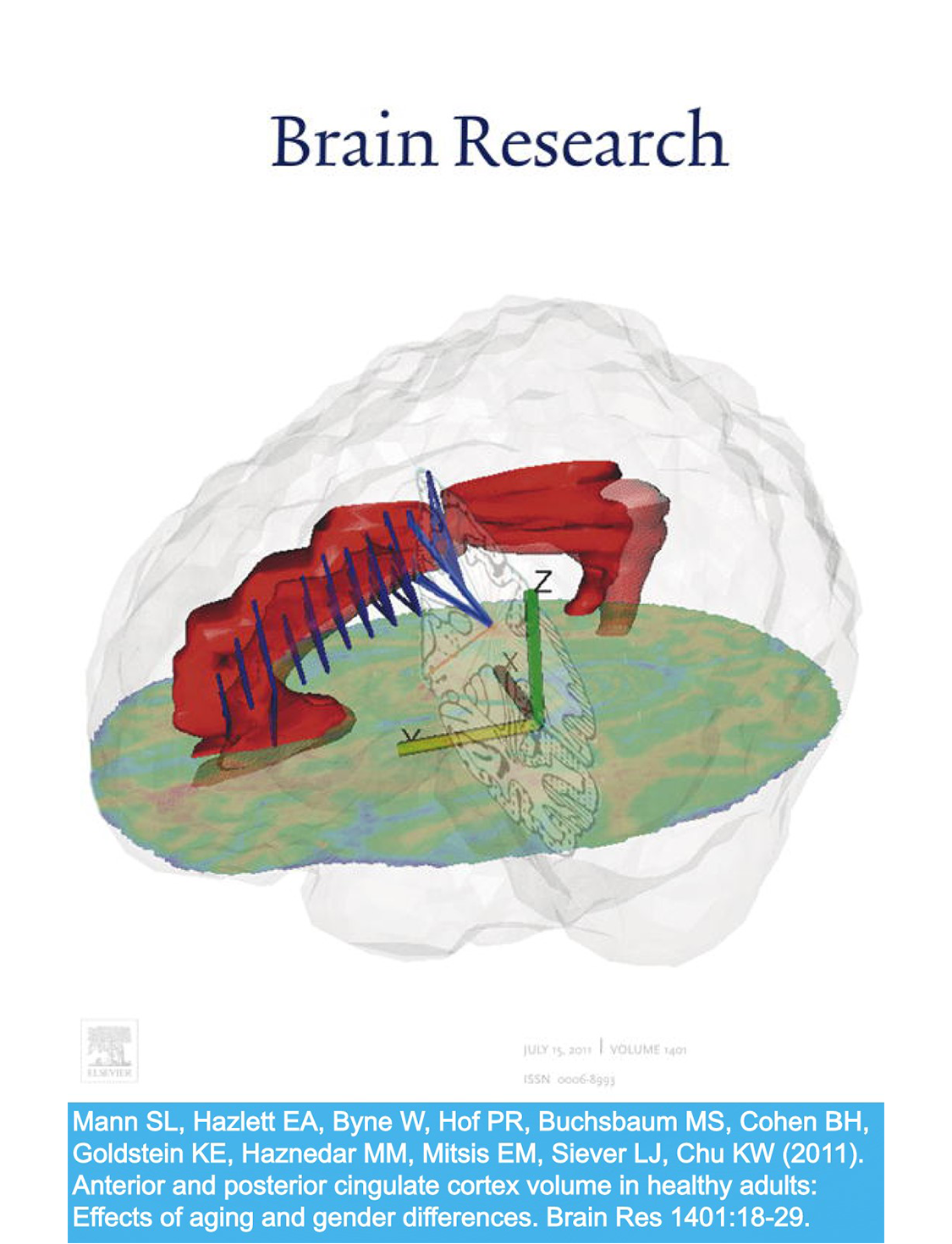
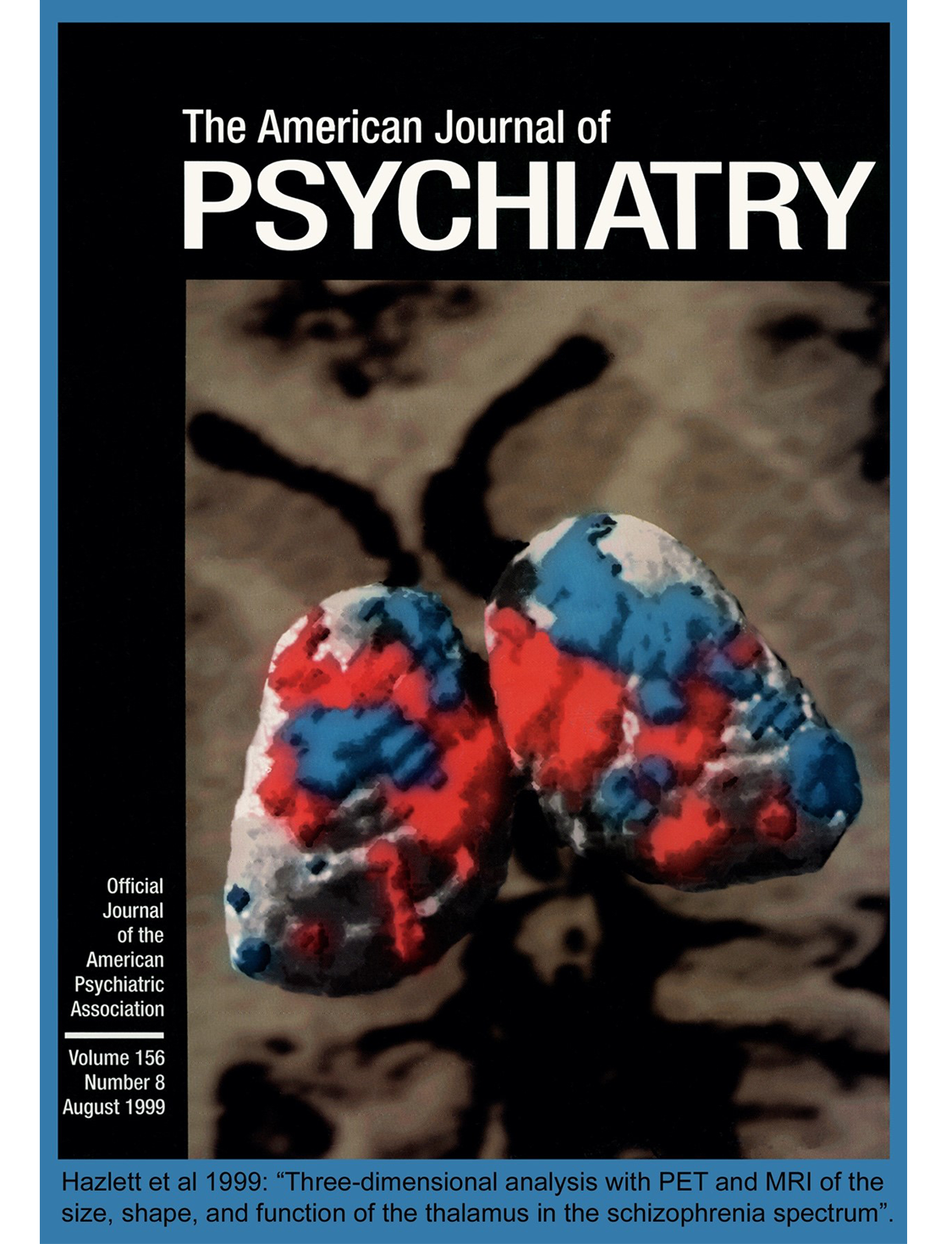
Dr. Hazlett is Principal Investigator on grants from the NIMH, the U.S. Department of Veterans Affairs, and the Department of Defense. She has received Young Investigator and Independent Investigator Awards from the Brain and Behavior Research Foundation (formerly NARSAD). Her work has been featured on the cover of three international journals (Biological Psychiatry, The American Journal of Psychiatry, and Brain Research). Professor Hazlett is a member of the Association for Psychological Research, Society for Psychophysiological Research, and the Society for Research in Psychopathology.

Current Projects and Awards
4/1/20 – 3/31/25 | Principal Investigator: NIMH R01 MH121411 (Total Award: $4,014,797)
“Longitudinal neuroimaging and neurocognitive assessment of risk and protective factors across the schizophrenia spectrum”
MPI: Phil Szeszko, Ph.D.
This research utilizes longitudinal multimodal MR imaging and Research Domain Criteria (RDoC) investigational approaches across schizophrenia-spectrum disorders to identify aberrant neural circuitry along a continuum from healthy controls to schizotypal personality disorder to recent-onset schizophrenia and examines changes in these measures over time in relationship to impairments in symptom severity, neurocognition, and functional outcome.
7/1/21 – 3/31/25 | Principal Investigator: NIMH R01 MH121411-02S1 Supplement (Total Award: $826,644)
“Longitudinal neuroimaging and neurocognitive assessment of risk and protective factors across the schizophrenia spectrum”
MPI: Phil Szeszko, Ph.D
This supplement leverages the parent R01 project to use advanced computational speech analytic approaches to identify the linguistic basis—semantics and syntax—that underlies language production along a spectrum from normal to gradations of thought disorder across the schizophrenia spectrum.
4/1/20 – 3/31/24 | Principal Investigator: Collaborative VA Merit I01 CX002093 (Total Award: $1,097,524)
“CTBI: Traumatic brain injury-induced inflammation effects on cognitive evaluations and response inhibition: Mechanisms of increased risk for suicidality”
MPI: Marianne Goodman, M.D.
This highly-collaborative research involves four VA sites. Our site at the JJP VA investigates brain activity with fMRI during cognitive and motor impulsivity tasks in Veterans with and without a history of mild traumatic brain injury (mTBI) and suicide attempt history. The Indy VA site (PI: Niculescu) will conduct the same impulsivity tasks in Veterans and also conduct all analyses on the blood. The New Jersey VA site (PI: Beck) will employ the same impulsivity tasks in animal models of mTBI. The study’s clinical core involves the Denver MIRECC and the NJ VA (Brenner & Interian).
4/1/18 – 3/31/23 | Principal Investigator: 1 IK6 CX001738 (Total Award: $905,806)
“VA CSR&D Research Career Scientist Award”
This award provides full-time VA salary support for the PI and enhances opportunities for (a) conducting collaborative neuroimaging and psychophysiological research, and (b) research mentoring at the JJPVAMC.
1/1/22 – 12/31/23 | Principal Investigator: VA RR&D SPiRE Grant RX003738 (Total Award: $229,809)
“A novel cognitive remediation intervention targeting poor decision making and depression in Veterans at high risk for suicide: A safe, telehealth approach during the COVID-19 pandemic”
This is a proof-of-concept study examining a novel cognitive remediation intervention that will be conducted virtually in 36 Veterans at high risk for suicide.
4/1/20 – 3/31/24 | Co-Investigator: VA CSR&D Merit Award I01 CX002039 (Total Award: $1,207,848)
“Predicting suicidal behavior in Veterans with bipolar disorder using behavioral and neuroimaging based impulsivity phenotypes”
PI: Phil Szeszko, Ph.D.
This project examines both trait and state measures of impulsivity in Veterans with bipolar disorder using self-report measures and fMRI to predict the occurrence of suicidal behavior longitudinally over one year.
10/1/18 – 9/30/23 | Co-Investigator: VA CSR&D Merit Award I01 CX001705 (Total Award: $1,629,240)
“Group (“Project Life Force”) vs. individual suicide safety planning RCT”
Principal Investigator: Marianne Goodman, M.D.
This project evaluates the effectiveness of a 10-session suicide safety planning group-based intervention for suicidal Veterans incorporating emotion regulation skills vs. safety planning without group involvement.
1/1/20 – 12/31/24 | Co-Investigator: VA CSR&D Merit Award I01 CX001980 (Total Award: $979,570)
“Reward processing and depressive subtypes: Identifying neural biotypes related to suicide risk, resilience, and treatment response”
PI: Susanna Fryer, Ph.D. (VAMCSF and UCSF; Early career investigator).
This project aims to evaluate neurobehavioral mechanisms involved in reward processing that contribute to reward and related deficits (anhedonia and amotivation) in depression using a multimodal approach (EEG, behavioral assessments, fMRI). The study will investigate the heterogeneity of depression— specifically in terms of reward-related brain functions and their clinical correlates.
1/1/20 – 12/31/23 | Co-Investigator: NIMH R21 MH119530 (Total Award: $480,000)
“Mapping treatment components to targets in Dialectical Behavior Therapy”
PI: Kathryn Dixon-Gordon, Ph.D. (UMass Amherst; Early career investigator).
This project uses behavior tasks and psychophysiology to probe treatment targets in patients with borderline personality disorder receiving DBT.
4/1/22 – 3/31/24 | Mentor: VA CSR&D Research Supplement to Promote Diversity I01 CX-22-029-01 (Total Award: $85,000)
“Impulsivity and suicide disclosure”
Principal Investigator: Robert Lane, Ph.D.
This Diversity Supplement involves mentorship of Dr. Lane who will use some of the data I have collected from my current VA Collaborative Merit Award to examine potential relationships between impulsivity and suicide disclosure.
7/1/20 – 6/30/25 | Mentor: NIMH T32 MH122394 (Total Award: $1,341,830)
“Training the next generation of clinical neuroscientists”
Principal Investigator: René S. Kahn, M.D., Ph.D.
I serve as a mentor in this fellowship program which is designed to train psychiatrists and clinical PhDs to formulate original research questions on etiology, pathogenesis, course, treatment and prevention of serious mental illness, with a focus on patients with schizophrenia and major mood disorders.
Publications
Laboratory Members
King-Wai Chu, PhD, Image Analyst
Education
BS in Aerospace Engineering, Polytechnic University
MS in Aeronautics and Astronautics, Polytechnic University
MS in Applied Math & Statistics, Stony Brook University
PhD in Applied Math & Statistics, Stony Brook University
Biography
Dr. Chu has been working with Dr. Hazlett for over 15 years. Dr. Chu is an expert in image processing of structural MRI, functional MRI, DTI and FDG-PET data. He has expertise in a variety of software packages used for neuroimaging data analysis including SPM, FSL, AFNI, Brain Voyager, E-Prime and DTI-Studio. He performs quality assurance upon image acquisition followed by image processing and analysis. He ensures that reliable data is acquired, optimizing signal-to-noise ratio for the key regions of interest in various research studies. Dr. Chu also maintains in-house software that Dr. Hazlett and her team use to trace regions of interest on structural MRI.

Kim Goldstein Zinn, PhD, Clinical Neuropsychologist
Education
BA, Princeton University
PhD in Clinical Psychology, Temple University
Biography
Dr. Zinn is a clinical neuropsychologist who specializes in the assessment and treatment of children, adolescents, and adults with a wide range of psychiatric and neurologic conditions. Dr. Zinn has published several peer-reviewed papers on emotion and cognition with Dr. Hazlett’s lab. Prior to joining Mount Sinai, Dr. Zinn was an Assistant Professor of Neuropsychology, Dept. of Psychiatry at Weill Cornell Medical College, and an Assistant Attending Psychologist at New York-Presbyterian Hospital.
Chi Chan, PhD, Clinical Psychologist
Education
BA in Psychology, Temple University
PhD in Clinical Psychology, University of Central Florida
Biography
Dr. Chan is a licensed clinical psychologist and Assistant Professor in the Department of Psychiatry at the Icahn School of medicine at Mount Sinai. She completed her Advanced Psychology Fellowship at the Mental Illness Research, Education, and Clinical Center (MIRECC VISN2) at the James J. Peters VA Medical Center. She has published work on neuroimaging and neuro-cognition in schizophrenia-spectrum disorders.

Katelyn Challman, PhD, Postdoctoral Fellow
Education
BA in Psychology, Point Loma Nazarene University
PhD in Clinical Psychology, Alliant International University in San Diego
Biography
Dr. Challman is a clinical psychologist completing her Advanced Psychology Fellowship at the Mental Illness Research, Education, and Clinical Center (MIRECC VISN 2). She is also a fellow in the Department of Psychiatry at the Icahn School of Medicine at Mount Sinai. Her primary research interests focus on neurocognitive functioning across the schizophrenia spectrum in relation to functional outcomes and overlapping obsessive-compulsive symptomology.

Terra Osterberg, BA, BS, Clinical Research Coordinator
Education
BA in Psychology, Wake Forest University
BS in Neuroscience, Wake Forest University
Biography
Terra has worked as a clinical research coordinator for Dr. Hazlett since February 2020. She primarily works on Dr. Hazlett’s collaborative VA Merit Study “CTBI: Traumatic brain injury-induced inflammation effects of cognitive evaluations and response inhibition: Mechanisms of increased risk for suicidality”, a multi-site project which combines neurobiological mechanistic studies in animals with human neuroimaging and biomarker analysis to understand the manner in which mTBI influences cognitive and behavioral impulsivity and suicidal behavior in veterans.

Sean Hollander, BA, Clinical Research Coordinator
Education
BA in Biological Sciences, Cornell University
Biography
Sean has worked as a clinical research coordinator for Dr. Hazlett since March 2022. He works on Dr. Hazlett’s five-year NIMH grant ”Longitudinal neuroimaging and neurocognitive assessment of risk and protective factors across the schizophrenia spectrum,” which uses fMRI and neurocognitive assessments to study schizophrenia spectrum disorders. He plans to pursue a career in medicine.

Education
BS in Neurobiology, Georgetown University
Biography
Kaitlyn has worked as a clinical research coordinator for Dr. Szeszko and Dr. Hazlett since October 2021. She works on their five-year NIMH grant, ”Longitudinal neuroimaging and neurocognitive assessment of risk and protective factors across the schizophrenia spectrum”, which uses fMRI and neurocognitive assessments to study risk and protective factors across the schizophrenia spectrum. Kaitlyn is currently pursing a Master’s degree for Biomedical Sciences with a concentration in Neuroscience at Icahn School of Medicine at Mount Sinai. She plans to pursue a career in medicine and complete a speciality in Neurosurgery.

Tasnova Ahmed, MA, Clinical Research Coordinator
Education
BA in Psychology, St. John’s University
MA in Psychology, St. John’s University
Biography
Tasnova has been working as a clinical research coordinator for Dr. Hazlett since October 2021. She works on finishing Dr. Hazlett’s four-year VA Merit study, “Neurobiology of Affective Instability in Veterans at Low and High Risk for Suicide,” which uses fMRI and psychophysiological measures to study suicidal behavior. She is concurrently working on starting Dr. Hazlett’s two-year pilot intervention study, “A Novel Cognitive Remediation Intervention Targeting Poor Decision-Making and Depression in Veterans at High Risk for Suicide: A Safe, Telehealth Approach During the COVID-19 Pandemic,” which aims to better understand Cognitive Remediation Therapy as a treatment for depression.

Collaborators
Mehmet Haznedar, MD
Education
MD, Ankara University Medical School
Residency in Psychiatry, Icahn School of Medicine at Mount Sinai
Biography
Dr. Haznedar is board-certified outpatient attending psychiatrist at the JJPVAMC and Assistant Clinical Professor at the Icahn School of Medicine at Mount Sinai. He has been in practice for over 25 years and has contributed extensively to clinical neuroimaging research throughout his career.

Philip Szeszko, PhD
Education
BS in Psychology, Stony Brook University
PhD in Clinical Psychology, St. John’s University
Biography
Philip R. Szeszko, Ph.D., is Associate Professor of Psychiatry at the Icahn School of Medicine at Mount Sinai and a Psychologist at the James J. Peters VA Medical Center. His main research interests focus on the use of magnetic resonance imaging to identify aberrant neurobiological mechanisms in patients with severe psychiatric disorders including bipolar disorder and psychosis. Dr. Szeszko has received grant funding from the National Institute of Mental Health, DANA Foundation, Brain and Behavior Research Foundation, Obsessive-Compulsive Foundation and American Foundation for Suicide Prevention. He has authored or co-authored over 130 peer-reviewed manuscripts and sits on the Editorial Boards of Progress in Neuro-psychopharmacology and Biological Psychiatry and Journal of the International Neuropsychological Society.

Marianne Goodman, MD
Education
MD, University of California – San Francisco School of Medicine
Residency, Clinical Psychiatry, University of California – San Francisco
Biography
Marianne S. Goodman, M.D. is a Professor of Psychiatry at The Mount Sinai School of Medicine. For the past 20 years she has also a worked as a full time VA clinical research physician at the James J. Peters VA (JJPVA). Her expertise is in the management of high risk suicidal and emotionally dysregulated Veterans, borderline personality disorder and delivery of dialectical behavioral therapy. More recently, she shifted her research direction to focus on treatment development for suicide prevention. Dr. Goodman designed “Project Life Force” (PLF) a novel group intervention that combines emotion regulation skills with suicide safety planning which was initially funded with a VA RR&D SPiRE pilot grant (2015-2017) and now recently funded for a multi-site RCT with a CSRD Merit (2018-2023). She also has an RR&D Merit (2017-2020) to further develop a dyad suicide safety planning intervention.
Recent Alumni
Nick Fernandez, MA
Education and Biography
BA in Psychology, Wake Forest University (2009)
MA in Psychology, New York University (2012)
Nick worked in Dr. Hazlett’s Lab from 2011-2013, and received a full scholarship to pursue a PhD in Clinical Psychology from Long Island University in Brooklyn.
Nick Blair, BA
Education and Biography
BA in Biochemistry, Skidmore College (2012)
Nick worked as a clinical research coordinator in Dr. Hazlett’s Lab from 2013-2015. He was primarily responsible for the psychophysiology components of Dr. Hazlett’s grants, which included both affective startle and prepulse inhibition (PPI) paradigms on a variety of psychiatric patients. He is pursuing an MD at Albert Einstein College of Medicine.
Michelle Feder, BA
Education and Biography
BA in Psychology, Columbia University (2012)
Michelle worked as a clinical research coordinator for Dr. Hazlett from 2012-2015. Michelle primarily worked on Dr. Hazlett’s 4-year VA MERIT study, “Selecting Best Treatment for Veterans with Schizophrenia,” which used fMRI and psychophysiological measures as potential predictors of treatment response. She is currently pursuing a PhD in clinical psychology at Yeshiva University.
Caitlin Kelliher, BA
Education and Biography
BA in Neuroscience & Behavior, Columbia University (2015)
Caitlin worked as a clinical research coordinator for Dr. Hazlett from 2015-2017. Caitlin worked primarily on Dr. Hazlett’s 4-year MERIT study, “White Matter Abnormalities in the Schizophrenia Spectrum,” which employed diffusion tensor imaging, structural MRI, and blood draws. She is currently working at a MedTech startup.
Nina Rose, MA
Education and Biography
BA in Psychology, University of Vermont (2013)
MA in Psychology, New York University (2019)
Nina worked as a clinical research coordinator for Dr. Hazlett from 2017-2019. She primarily worked on Hazlett’s 4-year VA Merit study, “Neurobiology of Affective Instability in Veterans at Low and High Risk for Suicide”, which employed fMRI and psychophysiology methodology to examine suicidal behavior in Veterans. She is currently pursuing PhD in clinical psychology at Yeshiva University.
Daniel Vaccaro, BA
Education and Biography
BA in Neuroscience & Behavior, Columbia University (2017)
Daniel has worked as a clinical research coordinator for Dr. Hazlett since June, 2017. He primarily works on Dr. Hazlett’s 4-year VA Merit study, “Neurobiology of Affective Instability in Veterans and Low and High Risk for Suicide,” which uses fMRI and psychophysiological measures to study suicidal behavior. He plans to pursue a career in medicine. He is currently pursuing an MD at Columbia University.
Elen-Sarrah Dolgopolskaia, BS
Education and Biography
BS in Biological Sciences with a Concentration in Neurobiology and Behavior, Cornell University (2020)
Elen-Sarrah has worked as a clinical research coordinator for Dr. Hazlett since June 2020. She primarily work on her five-year NIMH grant, ” Longitudinal neuroimaging and neurocognitive assessment of risk and protective factors across the schizophrenia spectrum”, which uses fMRI and neurocognitive assessments to study risk and protective factors across the schizophrenia spectrum. Elen-Sarrah will attend The American Medical School at Tel Aviv University in Fall 2022 with the intention of pursuing a speciality in either Psychiatry or Neurology.
Participant Recruitment
Within the JJPVAMC resides the Mental Illness Research Education and Clinical Center (MIRECC), which aims to generate new knowledge about the causes and treatments of mental disorders; apply new findings to model clinical programs; and widely disseminate new findings through education to improve the quality of veterans’ lives and their daily functioning in their recovering from mental illness. Presently, there are two laboratories within the MIRECC Department that are actively recruiting suitable participants for their studies.
Please see the flyers below and contact the phone number provided in order to further determine your eligibility. We thank you for your service!
Journal Covers
Left Cover: Hazlett EA, New AS, Newmark R, Haznedar MM, Lo JN, Speiser LJ, Chen AD, Mitropoulou V, Minzenberg M, Siever LJ, & Buchsbaum MS (2005). Reduced anterior and posterior cingulate gray matter in borderline personality disorder. Biol Psychiatry 58:614-623.
Middle Cover: Mann SL, Hazlett EA, Byne W, Hof PR, Buchsbaum MS, Cohen BH, Goldstein KE, Haznedar MM, Mitsis EM, Siever LJ, & Chu KW (2011). Anterior and posterior cingulate cortex volume in healthy adults: Effects of aging and gender differences. Brain Research 1401:18-29.
Right Cover: Hazlett EA, Buchsbaum MS, Byne W, Wei CT, Spiegel-Cohen J, Geneve C, Kinderlehrer R, Haznedar MM, Shihabuddin L, & Siever LJ (1999). Three-dimensional analysis with MRI and PET of the shape, size, and function of the thalamus in the schizophrenia spectrum. Am J Psychiatry 156:1190-1199.