Research
In the De Witte Lab we aim to understand how the immune system contributes to the development of psychiatric disorders, including schizophrenia, bipolar disorder, depression and autism. Although it is clear that these disorders are different from classical neuroinflammatory disorders, such as multiple sclerosis, there are several indications that the immune system contributes to them: First, large cohort studies have established epidemiological associations between psychiatric disorders and infections as well as autoimmune diseases. Second, genetic studies have found an association with immune-related genes. Third, changes in the expression of inflammatory genes and proteins have been found in blood, cerebrospinal fluid and brain tissue of patients with these disorders. How the immune system contributes to these orders at the mechanistic level is not yet clear. In our lab we aim to contribute to a better understanding of these mechanisms and to find novel immune-related targets to treat these disorders.

Contact Us
De Witte Laboratory
Department of Psychiatry
Projects
The role of microglia in psychiatric disorders
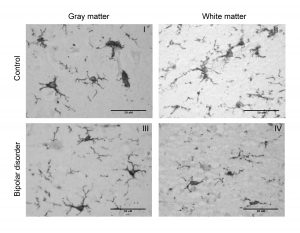
Understanding the role of microglia in psychiatric disorders is currently the main focus of our lab. Microglia are the main population of immune cells in the brain parenchyma. Microglia are known for regulating inflammation in the central nervous system. However, it is becoming more and more clear that these cells play also crucial roles when there is no inflammation. Microglia are important for shaping neuronal connections and regulation of neuronal functioning. Since altered neuronal connections and functioning is thought to underlie psychiatric disorders, dysfunction of microglia while performing these roles is hypothesized to contribute. We have set up several tools to study and characterize human microglia in health and pathology. We characterize their density and morphology in specific cortical layers (Figure 1) and we isolate them from post-mortem brain tissue for further characterization of the cells (Figure 2). The last years we have successfully isolated and characterized microglia from different brain regions from more >120 donors. These samples are used to investigate disease-related changes in microglia phenotype and function, as well as to analyze how genetic risk for neuropsychiatric disorder is related to gene expression (Figure 2). For further in-depth studies on changes in microglia function, in vitro cell models are needed. In our lab we have used advances of recent developments to culture microglia from monocytes and iPSCs and to generate cerebral organoids (Video and figure 3). We have optimized these models and with our colleagues in Utrecht the Netherlands, we were the first lab to describe a human cerebral organoid model in which microglia develop together with astrocytes and neurons. We use these models to study how genetic and environmental risk factors for psychiatric disorders change the phenotype and function of microglia and non-microglia cell types.
Infection and inflammation of the brain in psychiatric disorders

The association between the immune system and psychiatric disorders has been recognized for a long time. A role for the more classical immune-mediated mechanisms, including infections and inflammation of the brain, has been hypothesize to be involved in these diseases for decades. In our lab we have used novel virus discovery techniques and found no evidence for the presence of a specific virus in the cerebrospinal fluid or brain tissue in patients with schizophrenia. In addition, by using the formal criteria of neuroinflammation and postmortem brain tissue we found that most of the criteria for neuroinflammation are absent in bipolar disorder and schizophrenia.
Autoimmunity in psychiatric disorders

Autoimmune disorders have been reported to be more prevalent in patients with schizophrenia and bipolar disorder and their family members. In addition, it is known that antibodies that are produced against certain neuronal proteins, can cause an autoimmune encephalitis with prominent mood and psychotic symptoms. Autoimmunity has therefore been proposed as a potential underlying mechanism in a subgroup of patients with mood or psychotic disorders. If this would be the case, this would be very important for the diagnostic workup and treatment for this subgroup. However, whether this mechanism indeed plays a role in a subgroup of patients with a psychiatric diagnosis was still controversial. We investigated whether we could see more general sign of autoimmunity by measuring antinuclear autoantibodies (ANAs) and specific signs of autoimmunity of the brain by analyzing pathogenic neuronal auto-antibodies. We found that antibody-mediated autoimmunity is only rarely involved in psychotic disorders.
Meet the Team

Gijsje Snijders, MD,
PhD student/resident psychiatry
Gijsje is involved in several projects analyzing changes in microglia in postmortem brain tissue of patients with schizophrenia, bipolar disorder and major depressive disorder.
Frederieke Gigase, MSc
Associate researcher
Frederieke is the manager of the iPSC/organoid lab and involved in several organoid-based projects on the role immune processes in the pathogenesis of neuropsychiatric disorders.

Raphael Kübler, BSc
Master student
Raphael is involved in a project in which we aim to understand the role of microglia in schizophrenia with a focus on synaptic pruning.

Welmoed van Zuiden
Master student
Welmoed is involved in a project in which we analyze changes in microglia in postmortem brain tissue of patients with schizophrenia.

Amber Berdenis-van Berlekom, MSc
PhD student
Amber is enrolled in a PhD program at the UMC Utrecht, the Netherlands. She is interested in the role of microglia and astrocytes in neurodevelopmental disorders. In her PhD project, she studies the role of environmental exposure, including early life infections and malnutrition, on the development of cerebral organoids. She visits our lab to analyze cell-type specific changes in cerebral organoids.
Stephanie Gumbs
PhD student
Stephanie is involved in a PhD program at the UMC Utrecht, the Netherlands. She investigates the role of microglia in HIV infection. She visits our lab to isolate microglia from HIV-infected patients by collaborating with the Manhattan HIV Brain Bank and uses microglia cell models to study HIV infection of microglia in vitro.
Location
Annenberg 2584
Phone: 212-241-5067
Office: 212-241-5067
Lab: 212-241-4143
James.bieker@mssm.edu
Location
Annenberg 2584
Phone: 212-241-5067
Office: 212-241-5067
Lab: 212-241-4143
James.bieker@mssm.edu
