STRIDE: Study Targeting Recognition of Immune Deficiency and Evaluation
Icahn School of Medicine is a major referral center for infants, children, and adults, who have known or suspected primary immune deficiency diseases. We are taking the next step to help our patients, as well as those patients nationwide and globally by exploring new diagnosis and treatment therapies for these disorders. Researchers at Mount Sinai’s Human Immunodeficiency Diseases Laboratory launched STRIDE (Study Targeting Recognition of Immune Deficiency and Evaluation), which aims to evaluate data from patients with medical complications suggestive of immune deficiency to determine what immune systems may not be working normally. Our overall goal is to improve the quality of life for individuals with primary immune deficiencies. However a second agenda is to ensure that subjects with diverse racial and ethnic characteristics, are recognized in a large urban environment using our method of continuous computer screening of the medical record to identify patients with medical complications suggestive of immune deficiency. This study has been NIH funded since 2004.
Primary Immune Deficiency at Mount Sinai
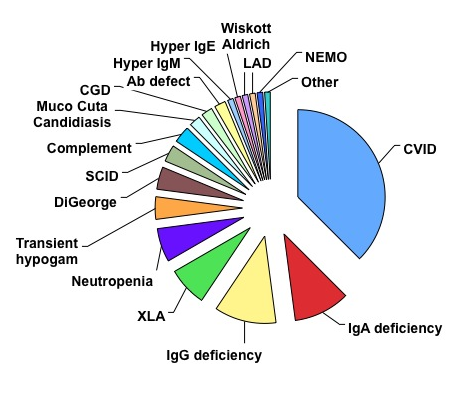
Some immune defects are more common than others. Icahn School of Medicine is a referral center for infants, children, and adults, who have known or suspected primary immune deficiency diseases. During recent years, more than 1000 patients have been seen and evaluated. Approximately one half are children and the other half are adult. As many studies have indicated, the most common immune defects involve deficient production of antibodies. Figure 1 shows the commonest defects seen in the last several years, based on percentages. Common variable immune deficiency, IgA deficiency, IgG subclass deficiency and transient hypogammaglobulinemia of infancy are some of the common immune defects that are associated with insufficient antibodies, but many other types of immune defects are also seen.
 Lack of Recognition of Primary Immune Deficiency
Lack of Recognition of Primary Immune Deficiency
Primary immune defects are believed to occur equally in all populations, races, and ethnic groups, but it has is very concerning that the diagnosis of primary immune defects patients varies considerably from one hospital to another and from one state to the next. For this reason, we have been investigating measures to enhance recognition and diagnosis of patients with primary immune defects at Mount Sinai area and developed an NIH-funded program based on a survey of the diagnoses of large patient groups to determine more about why this is so, and what measures can be taken to improve diagnosis.
A groundbreaking research investigation at Mount Sinai, entitled “STRIDE” contains several key elements. First we devised a method of performing a computer survey of all the diagnoses of patients admitted to Mount Sinai over time, to identify individual patients with medical diagnoses suggestive of immune deficiency, but who do not have another known reason for these illnesses (such as HIV cancer chemotherapy, debility, aging etc). These diagnoses (complied in the International Classification of Disease codes, Ninth Revision, ICD-9) are used to categorize every medical encounter, and are uniformly used by all physicians. Because the immune system plays an essential role in protecting against infections, many of the conditions that are associated with immune defects, involve infections of the nose, throat, skin, lungs or other organs. In addition, since the immune system is involved in the regulation of normal immunity, in some cases, the conditions that arise are autoimmune, or inflammatory.
Using these diagnostic codes for all these conditions, we developed a scoring algorithm to identify patients who had been given a diagnosis of two or more of the ICD- 9 coded complications associated with immunodeficiency. Using the same ICD codes, we also excluded all subjects with diagnoses that might lead to similar conditions, such as HIV, organ transplant, chemotherapy, etc. These ICD9 codes are also given relative rankings, to roughly indicate the severity of the conditions. These “score” or “report” cards give us an idea of the severity of the other conditions and suggest what kind of immune defect might be present. Using this system, we found that an ICD-9 based scoring algorithm identified patients who have had multiple illnesses suggestive of immunodeficiency; on testing these subjects, we found that this group contained undiagnosed and numerous minority patients with immunodeficiency. These results have been published.The conditions sought include:
Fever of unknown origin
Abnormal loss of weight/failure to thrive
Mycoses/Thrush/Candida
Otitis media: chronic
Sinusitis: chronic
Mastoiditis
Bronchitis: chronic
Pneumonia/Empyema/Lung abscess
Bronchietctasis
Chronic diarrhea
Malabsorption
Cellulitis
Osteomyelitis
Deep abscess: liver/spleen/rectal
Meningitis: aseptic/viral/bacterial
Septicemia
Lymphadenitis/lymph node enlargement
Splenomegaly
Autoimmune hemolytic anemia
Primary thrombocytopenia, ITP
Neutropenia
Lymphopenia
A second study was performed to record the kinds of illnesses that patients who were referred by other doctors to Mount Sinai for suspicion or confirmation of Primary Immune Deficiency. Over a two-year period, 237 patients were referred by internists, pediatricians, or allergists for suspected immunodeficiency. immunodeficiency was diagnosed 48%. Patients with immunodeficiency had a median score of 8 (interquartile range, 5 to 13), which was significantly higher (P 0.004) than the median score for those who did not have an immune deficiency (median score, 6; interquartile range, 3 to 10). Using age-adjusted comparisons, patients with immune deficiency also had a median score of 10 (interquartile range, 5 to 17.5), which was higher (P 0.025) than the median score of those without immune deficiency (median score, 8; interquartile range, 4 to 14). This study verified the use of the scoring parameters for locating patients with primary immune deficiency, and has been published.
We have also investigated the diagnosis of Primary Immune Deficiency in New York State using the Statewide Planning and Research Cooperative System (SPARCS) database, a comprehensive data reporting system that collects ICD-9 codes for each patient hospitalized in NYS. From 2000-2004 there were 13,539,358 hospitalizations for 4,777,295 patients; of these, 2,361 patients (0.05 %) were diagnosed with one or more of the ICD-9 codes for PID. Antibody defects were the most common diagnoses made. The PID population had significantly more Caucasians, and fewer African American or Hispanic subjects compared to the general population. Subjects with PID codes were younger, had longer hospitalizations, were less likely to have Medicare and more likely to have Medicaid or Blue Cross insurance. Most hospitalizations were due to respiratory and infectious diseases. Most patients resided in the most populous counties, Kings, New York and Queens, but the distribution of home zip codes was not proportional to county populations.
In ongoing studies we are also using the SPARCS dataset which collects ICD-9 codes for every hospital in and out patient encounter, complete demographics, home zip code, care locations, all services and charges in New York State. Patients are given a stable unique identifier so each can be identified through his/her multiple hospitalizations and all in and outpatient medical encounters. Included in each hospitalization are primary and up to 13 secondary ICD codes applied for the disease all complications experienced in that admission. This study was approved by the SPARCS Department of Health Review Board and will be used to further refine the ICD codes that are in used in the computer program. Our further plans will be to continue to refine the computer algorithm using the USIDNET data set, so that it may become a validated instrument for surveying electronic medical records.
Publications:
Cunningham-Rundles C, Sidi P, Estrella L, Doucette J. Identifying undiagnosed primary immunodeficiency diseases in minority subjects by using computer sorting of diagnosis codes. J Allergy Clin Immunol. 2004 Apr;113(4):747-55. PubMed PMID: 15100683.
Yarmohammadi H, Estrella L, Doucette J, Cunningham-Rundles C. Clin Vaccine Immunol. 2006 Mar;13(3):329-32. PMCID: PMC1391953 Recognizing primary immune deficiency in clinical practice.
Mehra A, Sidi P, Doucette J, Estrella L, Rouvelas H, Cunningham-Rundles C. Subspecialty evaluation of chronically ill hospitalized patients with suspected immune defects. Ann Allergy Asthma Immunol. 2007 Aug;99(2):143-50. PubMed PMID: 17718102.
Resnick ES, Bhatt P, Sidi P, Cunningham-Rundles C. Examining the use of ICD-9 diagnosis codes for primary immune deficiency diseases in New York State. J Clin Immunol. 2013 Jan;33(1):40-8. doi: 10.1007/s10875-012-9773-1. PubMed PMID: 22941512; PubMed Central PMCID: PMC3690548.
Sullivan KE, Puck JM, Notarangelo LD, Fuleihan R, Caulder T, Wang C, Boyle M, Cunningham-Rundles C. USIDNET: a strategy to build a community of clinical immunologists. J Clin Immunol. 2014 May;34(4):428-35. PubMed PMID: 24711005; PubMed Central PMCID: PMC4046905
