Overview
Our multidisciplinary research focuses on the psychosocial pathways involved in disease progression and recovery in drug addiction and related psychiatric disorders, namely stress and emotion-regulation related psychopathologies. A systems approach transcending brain-periphery-environment factors is used to examine how psychosocial processes relate with neurobiological correlates of behavior. Research is directed to advance understanding of: 1) how biomarkers associated with early adversity play lifelong roles in disease trajectory; 2) what are the impacts of adverse and protective psychosocial factors on brain structure and function in adults; and 3) what are the immune mechanisms that link between psychosocial factors and neurobiological markers. To investigate these questions, neuropsychological and behavioral assessments are used along with functional magnetic resonance imaging (fMRI), and analyzing peripheral biomarker assays. Through this work we seek to identify targetable mediators linking environment (stress) to psychiatric disorder and to facilitate the development of novel prevention strategies, diagnostic tools, and interventions.
Extending this line of study to advancement of treatment, in recent years our team has been working on the following initiatives: 1) for advancement of addiction medication development, we are the New York Site for a Randomized, Placebo-Controlled Trial of Extended-Release Naltrexone and Monthly Extended-Release Buprenorphine for Cocaine Use Disorder (Site PI: Bachi, Lead PIs: Trivedi & Shoptaw, CURB-2; NIDA UG1DA020024-18: CTN-109); 2) for evaluating the neurobiological effects underlying the ability of cannabidiol to reduce opioid craving, we conduct multiple clinical trials, including a NIDA UG3/UH3 DA050323– HEAL Initiative Clinical Trial (PI: Hurd, co-I: Bachi; titled, Cannabidiol in the treatment of opioid use disorder); on Brains Bioceutical Corp. Clinical Trial (PI: Hurd, mPI: Bachi; titled, Pharmacokinetic Investigation of BSPG Laboratories Cannabidiol in Healthy Participants); and a NIDA R01 DA048613 (PI: Hurd, co-I: Bachi; titled, Translating CBD Treatment for Heroin Addiction); 3) in collaboration with the Center for Biomedical and Population Health informatics at ISMMS, we built an AIMS-data warehouse, which integrates health data collected at the AIMS clinics and the health system in order to utilize big data via machine learning methods to predict and improve opioid treatments. In sum, we have the research experience, clinical expertise, established strong collaborative networks, and developed resources necessary to successfully design and lead rigorous randomized control clinical trials.

Keren Bachi, PhD, LCSW
keren.bachi@mssm.edu
212-585-4669
Lab location:
1399 Park avenue
New York, NY, 10029
Current Studies
Randomized, Placebo-Controlled Trial of Injectable Naltrexone and Monthly Injectable Buprenorphine for Cocaine Use Disorder (CURB-2)
Cocaine is one of the most commonly abused stimulants globally, and in the US, there are signs of a resurgence of cocaine use. A variety of pharmacotherapies for cocaine use disorder (CUD) has been explored but so far, no study has findings robust enough to warrant FDA approval. Recent research suggests that a kappa opioid receptor antagonist can curb the negative emotional states associated with stimulant withdrawal that leads to increased craving and drug-seeking behaviors. This protocol builds up on results of the Cocaine Use Reduction with Buprenorphine (CURB) study. It aims to evaluate the safety and efficacy of combined monthly injections of extended release naltrexone (XR-NTX) and injectable Buprenorphine (BUP) for Cocaine use disorder (CUD) compared to placebo.
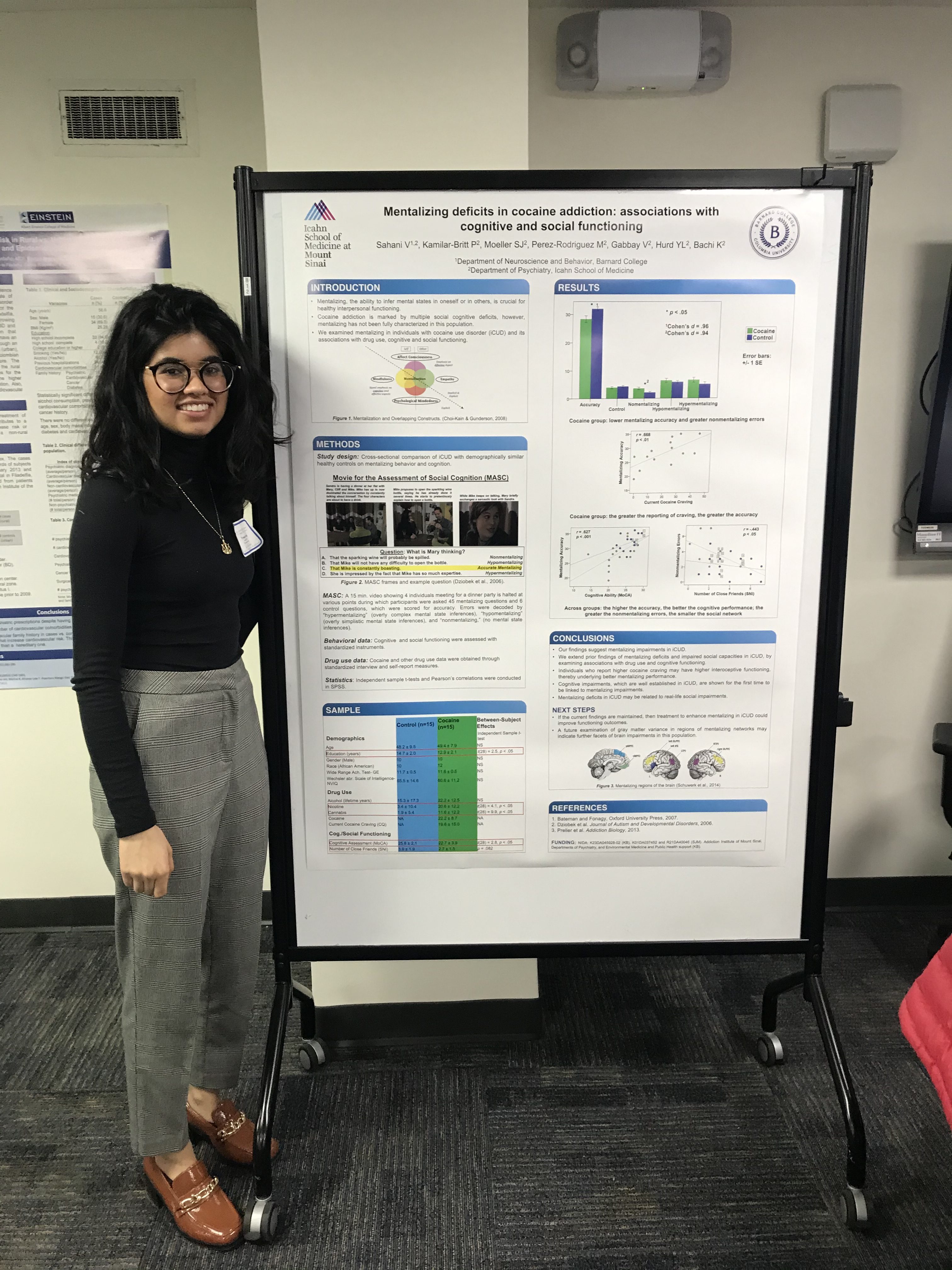
NIDA K23-DA045928-02 Patient-Oriented Career Development Award, Mentalizing deficits in cocaine addiction, associations with immune dysregulation and childhood maltreatment. Role: Principal Investigator
Drug addicted individuals frequently experience social stress (e.g., childhood maltreatment) which may impact interpersonal functioning, exacerbate illness risk (e.g., craving, relapse), and shape neural and physiological responses to stress. This study is aimed at characterizing these complex relationships by: (I) characterizing the behavioral and neural correlates of deficits in mentalizing in cocaine addicted individuals vs. matched healthy controls, using two well-validated functional magnetic resonance imaging paradigms that robustly activate the mentalizing network and characterization of Social Navigation; (II) comparing inflammation between the two study groups, using an immune-blood-profile previously associated with cocaine use, but here examined for the first time vis-à-vis mentalizing and childhood maltreatment; and (III) discerning whether inflammation markers mediate the relationships between childhood trauma with altered neural engagement/behavior during a novel mentalizing task. A better understanding of social cognitive impairments in cocaine addicted individuals, and particularly how they may be related to psychophysiological and social-environmental elements, may inform more effective treatment strategies, improving quality of life, and reducing societal burden.
Social Navigation in Cocaine Addiction in collaboration with Daniela Schiller, Ph.D.
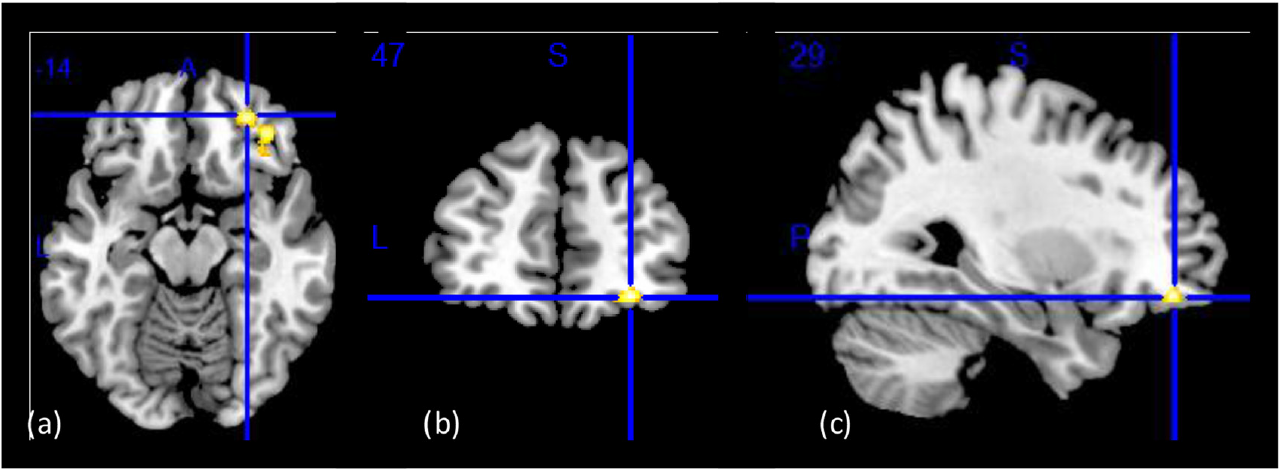
We have added to the K23 protocol an fMRI task that depicts a Map for Social Navigation for a comprehensive assessment of other social-cognitive factors that are beyond mentalizing. Social interactions can be framed by domains of power (being submissive or authoritative) and affiliation (sharing private information or intimacy), guided by episodic memory of prior social interactions. Revealing neural substrates of social interactions is complex because it is a dynamic phenomenon that requires consideration of ongoing changes in responses to social encounters. A well-validated and naturalistic fMRI paradigm, the Social Navigation task, has resulted in a two-dimensional geometric model of social interactions as shown by a ‘social space’ framed by power and affiliation in healthy individuals. Hippocampal brain activity predicted changes in subjective affiliation and power between people and fictional characters in a virtual role-playing game.
NIDA UG3/UH3 Clinical Trial 1UG3 DA050323-01 Principal Investigator: Yasmin Hurd, PhD; Co-Investigator: Keren Bachi, PhD, LSCW
Development of Medications to Prevent and Treat Opioid Use Disorders and Overdose. Cannabidiol in the treatment of opioid use disorder: A randomized, double-blinded, placebo-controlled study of pharmacological and long-term effects of Cannabidiol administration on opioid craving, relapse, and psychosocial functioning in individuals with opioid use disorder.
Lab Members

I am a neuroscientist whose rich clinical background set the stage for my scientific path. I am a Licensed Clinical Social Worker with more than a decade of psychotherapy experience treating adults with substance use disorders, and providing clinical supervision to clinicians in a range of clinical and managerial roles. Following the receipt of my
doctoral degree in 2014, I became the first Social Work Postdoctoral Fellow in Neuroscience at the Icahn School of Medicine at Mount Sinai (ISMMS). I completed a National Institute on Drug Abuse (NIDA) T32 postdoctoral fellowship in an interdisciplinary training linking neuroscience and systems therapeutics in drug abuse research,training with the Neuroimaging of Addiction and Related Conditions Research Program. In 2018 I was appointed Assistant Professor on the Investigator Track at the Departments of Psychiatry and Environmental Medicine and Public Health at ISMMS, and Faculty of the Addiction Institute of Mount Sinai (AIMS). I was awarded a NIDA K23 Mentored Patient-Oriented Research Career Development Award to examine neuroimmune underpinnings of social factors in cocaine addiction. In 2022 I was appointed Assistant Director of Clinical Research for AIMS, reflecting my role over the past few years in managing clinical trials involving medication development and neuroimaging.
My multidisciplinary research leverages my significant clinical and neuroscience experience in being centered on psychosocial pathways to disease and recovery in substance use disorders and related psychopathologies. A systems approach transcending brain-periphery-environment factors examines how psychosocial processes relate with neurobiological correlates of behavior. Through this work I seek to identify targetable mediators linking environment to psychiatric disorder and to develop prevention, diagnostic tools, and novel interventions. Extending this line of study to advancement of treatment, in recent years I have been contributing scientifically and by managing operations of the following initiatives: 1) for advancement of addiction medication development, I am the Site Principal Investigator for a Randomized, Placebo-Controlled Trial of Extended-Release Naltrexone and Monthly Extended-Release Buprenorphine for Cocaine Use Disorder (CURB-2; NIDA UG1DA020024-18: CTN-109); 2) for evaluating the neurobiological effects underlying the ability of cannabidiol to reduce opioid craving, I am a co-Investigator of multiple clinical trials, including a NIDA UG3/UH3 DA050323– HEAL Initiative Clinical Trial (PI, Hurd; titled, Cannabidiol in the treatment of opioid use disorder); mPrincipal-Investigator on Brains Bioceutical Corp. Clinical Trial (PI, Hurd; titled, Pharmacokinetic Investigation of BSPG Laboratories Cannabidiol in Healthy Participants); and a co-Investigator on a NIDA R01 DA048613 (PI, Hurd; titled, Translating CBD Treatment for Heroin Addiction); 3) in collaboration with the Center for Biomedical and Population Health informatics at ISMMS, we built an AIMS-data warehouse, which integrates health data collected at the AIMS clinics and the health system in order to utilize big data via machine learning methods to predict and improve opioid treatments. In sum, I have obtained the research experience, clinical expertise, established strong collaborative networks, and developed resources necessary to successfully design and lead rigorous randomized control clinical trials.









Former Lab Members

Vyoma Sahani
Clinical Research Coordinator

Philip Kamilar-Britt
Clinical Research Coordinator

Tien Tong
Postdoctoral Fellow

Vibhor Mahajan
PhD student

Julie Byrnes
MD/MPH student

Marybeth Nametz
Research Assistant

Cassandra B. Seltman
Research Assistant
Selected Publications
2023
-
Moazen-Zadeh, E., Chisholm, A., Bachi, K., Hurd, Y.L. (2023). Pharmacokinetics of Cannabidiol: A systematic review and meta-regression analysis. Cannabis and Cannabinoid Research. doi: 10.1101/2023.02.01.23285341 Accepted, Paper In-press
2022
-
Monti K.*, Bachi K.*, Gray M., Mahajan V., Sweeney G., Oprescu A., Hurd Y.L.**, and Lim S.** (2022). Datamining based clinical profiles of substance-use related emergency department utilizers: Rethinking emergency care. */** equally contributing authors. American Journal of Emergency Medicine . [doi: 10.1016/j.ajem.2021.12.059] [Epub ahead of print.] PMID: 35007871.
Shah-Mohammadi F., Cui W., Bachi K., Hurd Y.L., Finkelstein J. (paper accepted; conference 10.16-20.2022). Comparative Analysis of Patient Distress in Opioid Treatment Programs Using Natural Language Processing. The 7th International Conference on Informatics and Assistive Technologies for Health-Care, Medical Support and Wellbeing, HEALTHINFO 2022, Lisbon, Portugal. Conference paper. PMID: Not available.
Shah-Mohammadi F., Cui W., Bachi K., Hurd Y.L., Finkelstein J. (paper accepted; conference 7.11-15.2022). Using Natural Language Processing of Clinical Notes to Predict Outcomes of Opioid Treatment Program. The IEEE Engineering in Medicine & Biology Society (EMBC 2022) , Glasgow, UK. Conference paper. PMID: Not available.
Shah-Mohammadi F., Cui W., Bachi K., Hurd Y.L., Finkelstein J. (1.14.2022). Latent COVID-19 Clusters in Patients with Opioid Misuse. Stud Health Technol Inform 289: 123-127, Conference paper. [doi: 10.3233/shti210874] PMID: Not available.
Shah-Mohammadi F., Cui W., Bachi K., Hurd Y.L., Finkelstein J. (2.9-11.2022). Comparative Analysis of Patient Distress in Opioid Treatment Programs Using Natural Language Processing. 15th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC): Special Sessions – SERPICO 2022. Conference paper. PMID: Not available.
Sahani V., Hurd Y.L., Bachi K. Neural underpinnings of social stress in substance use disorders. (2022). (Sinha R., & Klaus M., Volume Editors). Neuroscience of Social Stress Volume, Current Topics in Behavioral Neurosciences Series , published by Springer. [PMID: 34971448] [doi: 10.1007/7854_2021_272.] [Epub ahead
of print]. PMID: 34971448
2020
- Moeller S.J., Kundu P., Bachi K., Maloney T., Malaker P., Parvaz M.A., Alia-Klein N., London E.D., Goldstein R.Z. (2020). Self-awareness of problematic drug use: Preliminary validation of a new fMRI task to assess underlying neurocircuitry. Drug and Alcohol Dependence, 1;209:107930. doi: 10.1016/j.drugalcdep.2020.107930. Epub 2020 Feb 28. PMID: 32145661
- Parish-Plass N., and Bachi K. (2020). Psychodynamic Animal-Assisted Psychotherapy: Processing and Healing through Relationships. In: Driscoll, C. (Ed.). Animal-Assisted Interventions for Health and Human Service Professionals. Nova Science Publishers, Inc. (NOVA), New York, NY.
2019
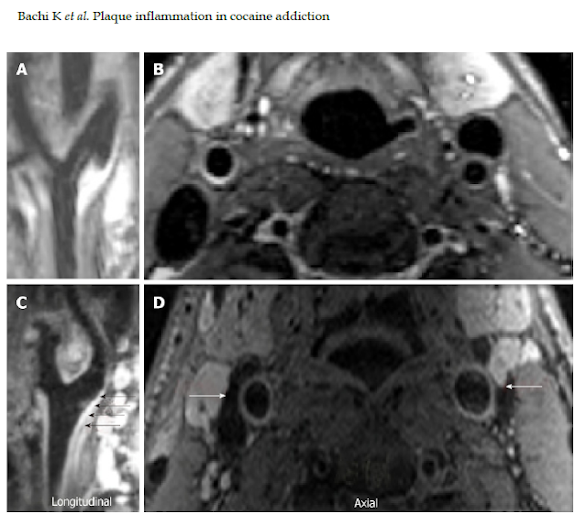
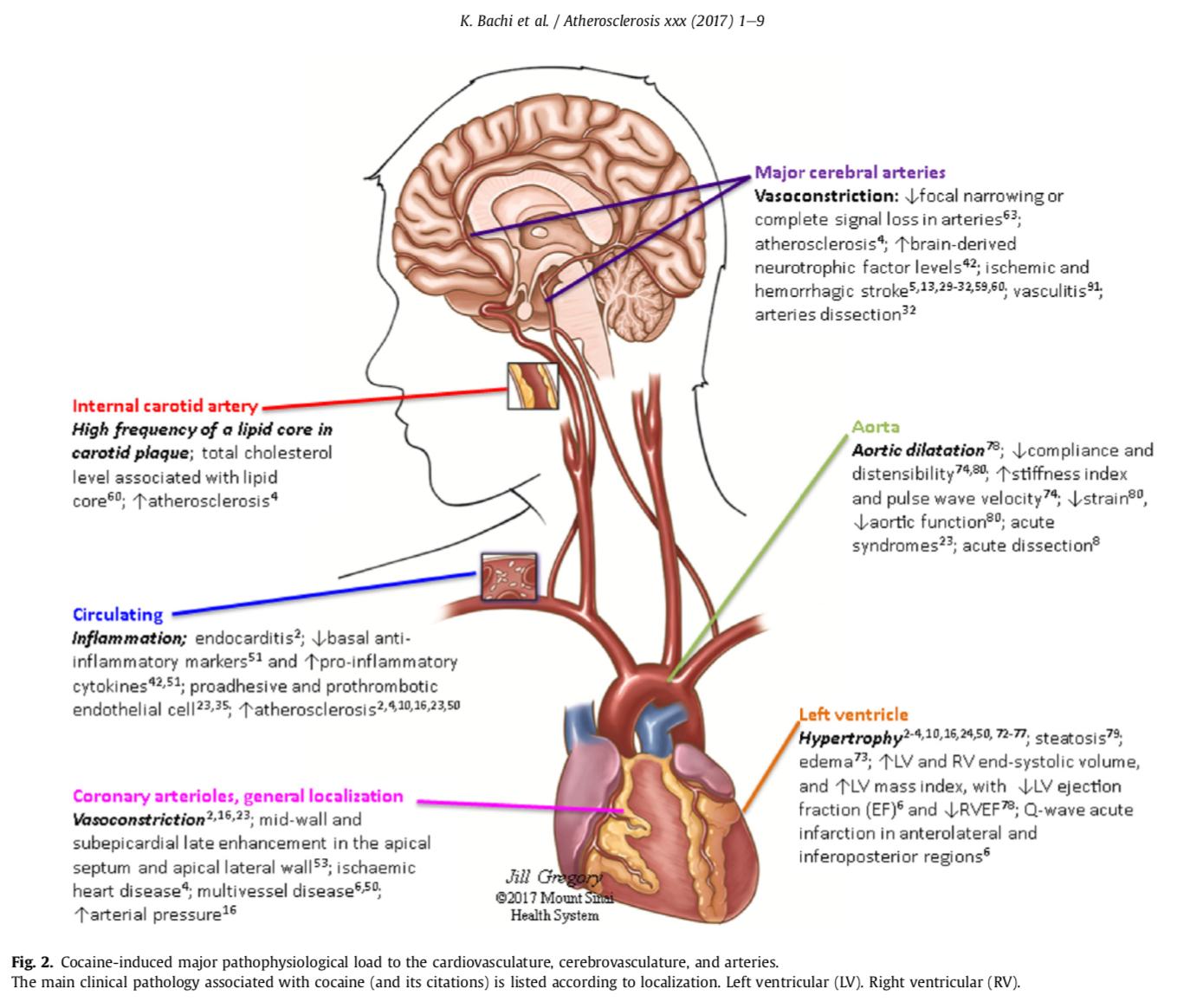
- Bachi K., Mani V., Kaufman A.E., Alie N., Goldstein R.Z., Fayad Z.A, Alia-Klein N. (2019). Imaging plaque inflammation in asymptomatic cocaine addicted individuals with simultaneous PET/MR Imaging. World Journal of Radiology;11(5):62-73. [PMID: 31205601] [DOI: 10.4329/wjr.v11.i5.62].
- Colicino E., Hazeltine D., Schneider K.M., Zilverstand A., Bachi K., Alia-Klein N., Goldstein R.Z., Todd A.C., Horton M. (2019). Cocaine addiction severity exacerbates the negative association of lifetime lead exposure with blood pressure levels: Evidence from a pilot study. Environmental Disease, 4(3):75-80. [PMID: [DOI: 10.4103/ed.ed_21_19].
- Agurto C., Norel R., Pietrowicz M., Parvaz M.A., Kinreich S., Bachi K., Cecchi G., Goldstein R.Z. Speech Markers for Clinical Assessment of Cocaine Users. (2019). IEEE Xplore Open Preview, Paper presented at: ICASSP 2019 – 2019 IEEE International Conference on Acoustics, Speech and Signal Processing (ICASSP); 12-17 May 2019, 2019.
2018
- Bachi K., Parvaz M.A., Moeller S.J., Goldstein R.Z., Alia-Klein N. (2018). Reduced orbitofrontal gray matter concentration as a marker of premorbid childhood trauma in cocaine use disorder. Frontiers in Neuroscience. doi: 10.3389/fnhum.2018.00051
- Alia-Klein N., Preston-Campbell R.N., Moeller S.J., Parvaz M.A., Bachi K., Gan G., Zilverstand A., Konova A.B., Goldstein R.Z. (2018). Trait anger modulates neural activity in the fronto-parietal attention network. Plos One. 13(4): e0194444.
- Moeller S.J., Zilverstand A., Konova A.B., Kundu P., Parvaz M.A., Preston-Campbell R.N., Bachi K., Alia-Klein N., Goldstein R.Z. (2018). Neural correlates of drug-biased choice in individuals with current and former cocaine use disorder. Biological Psychiatry: Cognitive Neuroscience and Neuroimaging, 3(5): 485-494.
2017
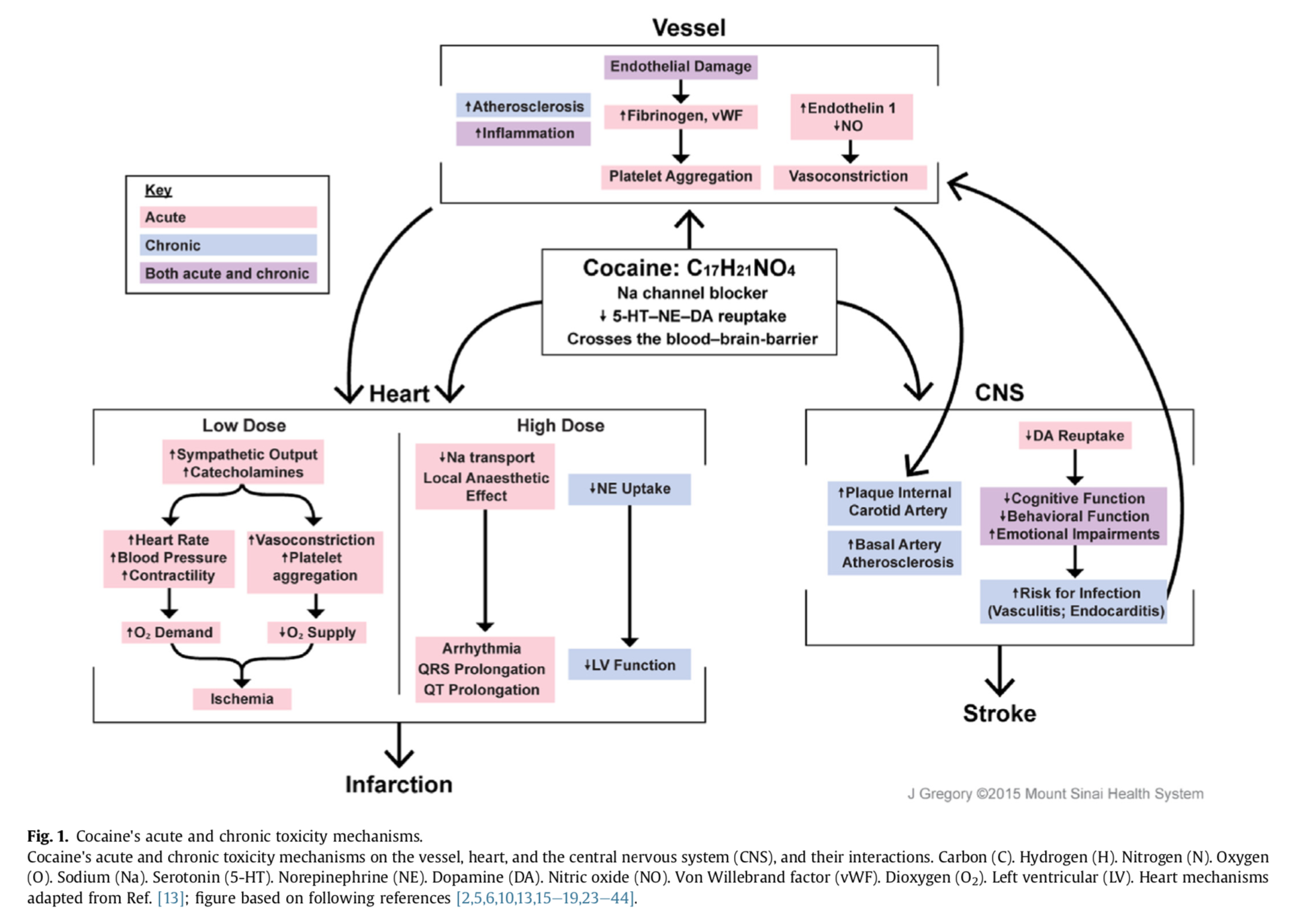
- Bachi K., Mani V., Jeyachandran D., Fayad Z.A, Goldstein R.Z., Alia-Klein N. (2017). Vascular disease in cocaine addiction. 262(Jul): 154-162. doi: http://dx.doi.org/10.1016/j.
- Bachi K., Mani V, Trivieri MG, Jeyachandran D, Fayad ZA, Goldstein RZ, Alia-Klein N. (2017). Reply to: “β-blocker treatment of vascular disease in cocaine addiction”. 264(Sep): 123–124. doi: https://doi.org/10.1016/j.atherosclerosis. 2017.07.012
- Bachi K., Sierra S., Volkow N.D., Goldstein R.Z., Alia-Klein N. (2017). Is biological aging accelerated in drug addiction? Current Opinion in Behavioral Science, 13, 34-39. doi: 10.1016/j.cobeha.2016.09.007
2016
- Bachi K., Parish-Plass N. (2016). Animal-assisted psychotherapy: A unique relational therapy for children and adolescents (Editorial). Clinical Child Psychology and Psychiatry. doi: 10.1177/1359104516672549
2013
- Bachi K. (2013). Application of Attachment theory to equine-facilitated psychotherapy. Journal of Contemporary Psychotherapy, 43(3), 187-196, first published on March 14, 2013. doi: 10.1007/s10879-013-9232-1
- Bachi K. (2013). Equine-facilitated prison-based programs within the context of prison-based animal programs: State of the science review. Journal of Offender Rehabilitation, 52(1), 46-74. doi:10.1080/10509674.2012.734371
2012
- Bachi K., Terkel J., Teichman M. (2012). Equine-facilitated psychotherapy for at-risk adolescents: The influence on self-image, self-control and trust. Clinical Child Psychology and Psychiatry, 17(2), 298-312, first published on July 14, 2011. doi: 10.1177/1359104511404177
- Bachi K. (2012). Equine-Facilitated Psychotherapy: The gap between practice and knowledge. Society and Animals, 20(4), 364-380. doi: 10.1163/15685306-12341242
2010 & Older
- Bachi K. (2000). The contribution of therapeutic horseback riding to substance abusers. Animals & Society, 11, 20-26 (Hebrew).
- Bachi K. (2004). Summing of CIAS conference of March 28th, 2004, Penn. Uni., PA: Animal assisted interventions for adolescents with mental illness. Animals & Society, 25, 27-29 (Hebrew).
- Bachi K., Terkel J., Teichman M. (2007). Equine-facilitated psychotherapy for at-risk adolescents: The influence on self-image, self-control and trust. Mifgash, Journal of social- educational work, 26, 137-154 (Hebrew).
- Bachi K. (2007). Equine-facilitated evaluation. Animals & Society, 33, 54-62 (Hebrew).
Oral Presentations
-
Bachi K. (5.30-6.2.2023). Setting the Stage for Personalizing Treatment of Substance Use Disorder: Neuro-Psychosocial Determinants. Panel title: Drug Discovery and Precision Medicine Approaches to Reduce Clinical Burden of Substance Use Disorders (Trivedi M, Chair). 2023 Annual Meeting of the American Society of Clinical
- Schafer M., Kamilar-Britt P., Moeller S.J., Gabbay V., Hurd Y.L., Schiller D., Bachi K. (4.24.2020). The hippocampus encodes 2D social distances. Oral presentation. The Friedman Brain Institute 12th Annual Neuroscience Retreat 2020. The Icahn School of Medicine at Mount Sinai, New York, NY.
- Bachi K. (04.06.2020). Mixed methods research: PhD dissertations and healthcare studies. PhD Dissertation Seminar, The Graduate Center of the City University of New York, The Silberman School of Social Work at Hunter College, New York, NY.
- Bachi K., and Salsitz E. (2.7.2020). Staging and stratified approach to addiction disease and treatment: Work in progress. 2020 Intersection of Science, Treatment and Policy Conference, New York Society of Addiction Medicine, New York, NY.
- PANEL: Shaham Y. (Chair), Bachi K. (Co-Chair), Venniro M. (Presenter), Perini I. (Presenter), Bachi K. (Presenter), Rajita Sinha R. (Presenter). (12.09.2019). Recent Advances in the Role of Social Factors in Drug Addiction: Preclinical and Clinical Studies. 58th Annual Meeting of the American College of Neuropsychopharmacology (ACNP), Orlando, FL.
- AIMS kickoff event: Bachi K. (10.30.2019). The neurobiological impact of early childhood trauma. Confronting Addiction: Science, Policy, and Care. New York Academy of Medicine, Presented by the Addiction Institute of Mount Sinai.
- Bachi K. (10.30.2019). The neurobiological impact of early childhood trauma. Confronting Addiction: Science, Policy, and Care. New York Academy of Medicine, Presented by the Addiction Institute of Mount Sinai.
- Bachi K. (9.26.2019). The social connection: advances in addiction phenotyping. Emerging Addiction Science Workshop of the Division on Substance Use Disorders, Department of Psychiatry, Columbia University, New York.
- Bachi K. (5.16.2019). Psychosocial effects in addiction: structure, function, and putative underlying neuroimmune mechanisms. Presentation in Seminar of the Sussex Addiction Research & Intervention Centre, University of Sussex, Brighton, UK.
- Bachi K., Kundu P., Malaker P., Maloney T., Parvaz M.A., Alia-Klein N., Goldstein R.Z., Moeller S.J. (4.6.2018). Behavioral and neural mentalization deficits in cocaine use disorder. Oral presentation. 2018 New York Social and Affective Neuroscience Meet Up, Adelphi University, New York, NY.
- Bachi K., Mani V., Goldstein R.Z., Fayad Z., Alia-Klein N. (5.13.2015). Characterizing atherosclerosis in asymptomatic cocaine addicted individuals. Oral presentation. The Mount Sinai Neuroscience Annual Retreat 2015. The New York Academy of Medicine, New York.
- Bachi K. (1.15.2014). An Equine-Facilitated Prison Based Program: Effects on Recidivism. Oral presentation. The 2014 Annual Conference of the Society for Social Work and Research (SSWR), San Antonio, TX.
- Bachi K. (3.26.2010). Research study of Youth at Risk and EFP. Oral presentation. NARHA Region 2 Conference hosted by NYSTRO at Clearpool Education Center, Carmel, NY.
Psychopharmacology (ASCP) , Miami Beach, FL.
Bachi K. (10.19.2022). Setting the Stage for Personalizing Treatment of Substance Use Disorder: Neuropsychosocial Determinants. Presentation to the Department of Psychiatry , ISMMS, New York.
Bachi K. (12.8.2021). Psychosocial effects in addiction: structure, function, and putative underlying neuroimmune mechanisms. The Substance Use Disorders module of the didactic course for Postgraduate Psychiatry Residents Physicians in 2nd year, ISMMS.
Schafer M., Kamilar-Britt P., Sahani V., Bachi K., Schiller D*. (12.7.2021). Social Place Representation in the Human Hippocampus. The 60th Annual Meeting of the American College of Neuropsychopharmacology (ACNP), San Juan: Puerto Ricco.
Schafer M*., Kamilar-Britt P., Sahani V., Moeller S.J., Gabbay V., Hurd Y.L, Bachi K., Schiller D*. (11.9.2021). The hippocampus represents abstract social place: encoding and decoding evidence in independent samples. The 50th Annual Meeting of the Society for Neuroscience , Virtual meeting.
Bachi K. (7.1.2021). Advances in Addiction Pathways: Elucidating the Social Connection. The Division of General Medicine and Psychiatry monthly DGIM/PRIME meeting, Montefiore Medical Center, Albert Einstein College of Medicine , Bronx, New York.
Bachi K. (6.11.2021). Advances in addiction pathways: elucidating the social connection. Depression and Affective Neuroscience (DANS) meeting, ISMMS.
Bachi K. (6.3.2021). Advances in addiction pathways: elucidating the social connection. AIMS lecture series to the clinicians, AIMS, ISMMS.
Bachi K. (12.2.2020). Setting the stage for personalizing treatment of substance use disorder: neuro-psychosocial determinants. The Substance Use Disorders module of the didactic course for Postgraduate Psychiatry Residents Physicians in 2nd year, ISMMS.
Bachi K. (04.06.2020). Mixed methods research: PhD dissertations and healthcare studies. PhD Dissertation Seminar, The Graduate Center of the City University of New York, The Silberman School of Social Work at Hunter College, New York, NY.
If you are interested in our work and would like to inquire about research or educational opportunities, please email our principal investigator Dr. Keren Bachi at keren.bachi@mssm.edu
Postdoctoral Fellowship Opportunities:
Our lab is currently inviting applicants for a Postdoctoral Fellowship position in clinical neuroscience and social-cognitive neuroimaging. Directed by Keren Bachi, PhD, LCSW, our research group studies the neurobiological underpinnings of social factors in human drug addiction. We are seeking a highly motivated Postdoctoral Fellow, who will primarily assist with neuroimaging data analysis and in managing our NIH-funded research projects which utilize innovative neuroimaging, immunological, and clinical trial methodologies. The position is for a term of at least 2 years and has a flexible start date (could begin immediately). Interested candidates can click the participate in research button below.
Current Research Opportunities:We are currently recruiting for our studies. If you are interested in participating in one of our research studies, click the recruitment button below.
Psychosocial Neuroimmune Addiction Lab
1399 Park ave., New York, NY, 10029
212-585-4653